Dry Needling for Neck Pain
A long day at the computer tightens the base of the skull; turning the head while driving sends a sharp pull into the side of the neck; sleeping awkwardly creates stiffness that lasts for days. These patterns are extremely common.
Many cases of non-traumatic neck pain involve a muscle driven component: tight upper trapezius, overloaded levator scapulae, irritated scalenes, or trigger points in the suboccipitals that refer pain toward the head, neck, or upper back.
Dry needling for neck pain targets these muscular contributors. When the exam identifies trigger points reproducing a patient’s exact pain pattern, reducing that irritability may lower nociceptive drive and restore comfortable motion.
For a plain-language overview of what to expect, see the Dry Needling Guide and the Trigger Points Guide.
Key Points
Most suitable cases: neck pain with muscular cues—turning the head, looking down, desk work, driving, overhead activity, sleeping position sensitivity.
Primary effect: reduction of trigger-point activity in upper trapezius, levator scapulae, SCM, scalenes, suboccipitals, splenius cervicis, and semispinalis muscles.
Muscle coverage: upper trapezius, levator scapulae, SCM, scalenes, splenius capitis/cervicis, semispinalis, suboccipitals, rhomboids, serratus posterior superior, and thoracic erector spinae.
Timeline: many individuals notice early change within 1–3 sessions; a short course of 4–6 visits is common.
Practical trial: 3–5 sessions with graded progression.
Session pacing: conservative dose at first, expanding as comfort increases.
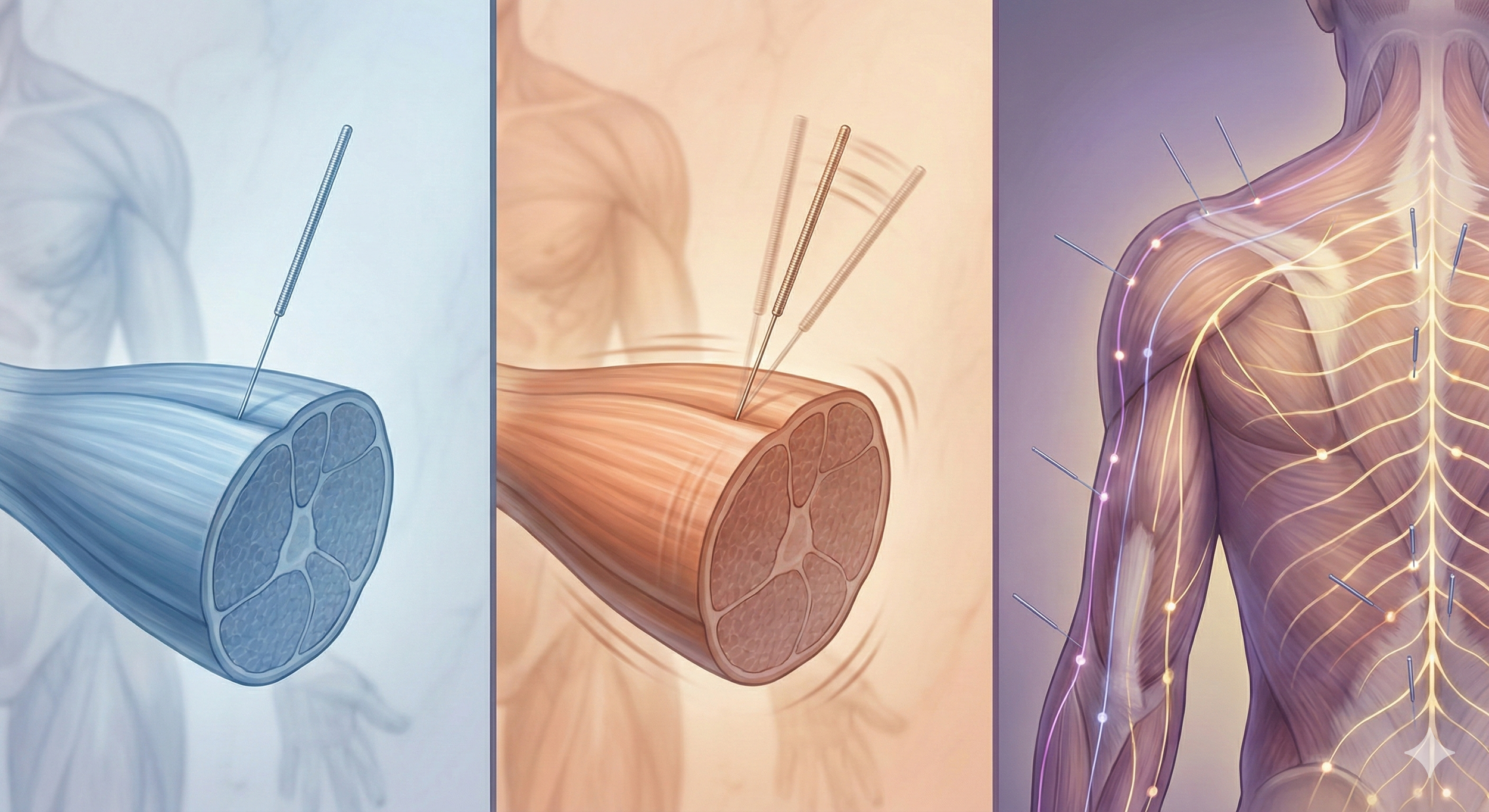
Dry needling for neck pain infographic
Neck Pain: Brief Condition Overview
Neck pain is one of the most common musculoskeletal complaints, often influenced by posture, movement patterns, stress, and sleep position. A significant number of cases involve muscles that refer pain to the neck, shoulder, or head, creating patterns that feel deeper or more painful than the underlying tissue damage would suggest.
Signs & symptoms (common features):
Pain turning the head or looking down
Upper trapezius tightness or “hard knots”
Temple, behind-the-eye, or base-of-skull pain
Pain radiating into the upper back or shoulder
Stiffness after long periods of sitting, driving, or screens
Pain that fluctuates more with posture than with activity level
Typical treatment options include:
Posture and workstation adjustments
Strengthening of deep neck flexors and scapular stabilizers
Soft-tissue release and mobility work
Dry needling to reduce muscle-driven nociception
Sleep-position strategies and activity modification
How Muscle Pain Can Mimic Orthopedic or Neurologic Neck Conditions
Muscle-driven neck pain frequently resembles more serious conditions. Trigger points in the upper trapezius, levator scapulae, SCM, splenius muscles, and scalenes can reproduce:
Headaches
Pain behind the eye
Shoulder or upper-back pain
“Nerve-like” tingling from muscle referral
Sharp pain when turning the head
Pain radiating down the shoulder blade
Pain that feels like a “pinched nerve”
Because these referral patterns follow predictable maps, muscular neck pain can feel like:
Cervical disc irritation
Nerve impingement
Thoracic outlet syndrome
Shoulder dysfunction
Whiplash carryover
Occipital neuralgia
Muscle referral often creates deep, spreading, or traveling pain that patients interpret as a disc issue or nerve problem—even when imaging is normal.
Why this matters clinically
Muscle referral can:
Produce sharp or pinpoint neck pain with rotation
Create headaches that mimic migraine or tension patterns
Cause neck stiffness that feels “joint-based”
Limit range of motion more than true structural injury
Mimic nerve symptoms without nerve compression
Fluctuate with posture or stress rather than with activity load
Dry needling helps differentiate these patterns. When symptoms improve after releasing specific muscles—SCM, traps, levator, scalenes, or suboccipitals—it strongly suggests a muscular source rather than a cervical disc or nerve-root lesion.
Neck Pain Patterns & Associated Trigger Points
Pain turning the head (rotation pain)
Pain at the base of the skull
Pain radiating into the shoulder or upper back
Pain behind the eye, temple, or forehead
Pain with looking down (text neck pattern)
Cervical extensor group
Neck Pain Trigger Points
The muscles below are frequently involved when neck pain is driven by postural load, rotation restrictions, or head-supported movement. Each is listed once with a brief referral pattern to guide focused palpation and treatment planning.
Upper Trapezius
Referral: Temple, jaw angle, side of head, and upper neck; often flares with desk work and stress.
Levator Scapulae
Referral: Upper neck and superior angle of scapula; common when rotation is painful.
Sternocleidomastoid (SCM)
Referral: Forehead, eye region, temple, cheek; associated with dizziness or “band-like” head tension.
Scalenes
Referral: Side of neck, top of shoulder, upper chest, and arm; can mimic nerve symptoms.
Suboccipitals
Referral: Base of skull, eye region, forehead; strongly involved in posture-related headaches.
Splenius Capitis
Referral: Top of head, posterior skull, and behind the eye; often worsens with rotation.
Splenius Cervicis
Referral: Upper neck and shoulder blade; commonly irritated by turning the head.
Semispinalis
Referral: Skull base, upper neck, and back of head; connected to neck stiffness with looking down.
Rhomboids
Referral: Between the shoulder blades; often involved in posture-related upper back pain.
Serratus Posterior Superior
Referral: Upper back and medial scapula border; may present as “knot-like” tightness.
For complete referral maps and exam guidance, visit the Trigger Points Guide and the Dry Needling Guide.
How Dry Needling Fits Neck Pain With Upper Trapezius, Levator, SCM & Suboccipital Drivers
Dry needling for neck pain is most relevant when symptoms follow muscle-driven patterns: stiffness after sitting, pain on rotation, tension at the skull base, or radiating pressure toward the temple or upper back. In these cases, hyper-irritable trigger points in the upper trapezius, levator scapulae, scalenes, SCM, splenius muscles, semispinalis, and suboccipitals can refer pain directly into the neck or head.
These trigger points may:
Increase upper neck tension
Limit rotation, flexion, or side-bending
Create headaches or eye-region pressure
Mimic nerve pain into the upper back or shoulder
A thin filiform needle is used to release the specific neuromuscular points identified on examination. It’s common to feel a deep ache, a brief twitch, or a familiar line of pain that radiates toward the temple, skull base, or upper back. These responses often indicate accurate targeting.
Sessions begin with a modest dose and progress gradually based on sensitivity and post-visit response. By dampening overactive muscles in the neck and upper back, dry needling can reduce background muscle tone, improve range of motion, and lower the mechanical load on the cervical spine.
For an overview of session flow and technique, see the Dry Needling Guide.
What to Expect in a Session (Comfort, Pacing, Soreness)
A session begins with a review of symptom onset, and trying to gather an understanding of what makes things better or worse. The neck and shoulder are assessed for mobility, strength, and reproduction of familiar pain. Palpation guides muscle selection and dosing.
Clients often feel a deep ache or brief twitch during needling; these sensations tend to settle quickly. Post-session soreness may feel workout-like and can last 24–72 hours. Light mobility and hydration help this resolve smoothly.
Relief Timeline & Visit Cadence
Early change: within 1–3 sessions, improvements in pain, sleep (if affected), and general load tolerance
Short series: 4–6 visits for more sustained improvement
Chronic cases: long-standing patterns or layered muscular drivers may require 10+ visits or maintenance
A 3–5 session trial helps determine responsiveness. If symptoms don’t shift, the muscle sequence, dosing strategy, or loading plan is revised.
Dry Needling for Neck Pain Research
Dry needling for neck pain is supported by recent systematic reviews and randomized trials showing short- to mid-term pain reductions, especially when used within a multimodal physical therapy program, although not all studies show added benefit over high-quality comparison care. Overall, effects appear strongest for short-term pain, disability, pressure-pain sensitivity, and selected cervical range-of-motion outcomes.
Systematic Review & Meta-Analysis: Dry Needling for Chronic Neck Pain (2023)
A 2023 systematic review and meta-analysis of 14 randomized controlled trials found that dry needling improved pain intensity and functional capacity in adults with chronic neck pain at short- and mid-term follow-up compared with other interventions or sham, with greater benefits when combined with physical therapy modalities such as stretching, manual therapy, or exercise. Across studies, dry needling was applied to posterior cervical and shoulder-girdle muscles (commonly upper and lower trapezius, levator scapulae, splenius, and cervical multifidi) over 1–6 sessions, consistently increasing pressure pain thresholds and reporting no serious adverse events, while long-term results beyond three months were more mixed and sometimes favored alternative techniques such as miniscalpel-needle or electrotherapy.
Trigger Point Dry Needling for Acute Mechanical Neck Pain: Randomized Clinical Trial (2014)
A single-blind randomized clinical trial in 17 patients with acute mechanical neck pain compared one session of trigger point dry needling of active upper trapezius trigger points against a waiting-list control. The dry needling group demonstrated greater immediate and 1-week reductions in neck pain, larger increases in local and widespread pressure pain thresholds, and improved cervical range of motion, with between-group effect sizes reaching medium to large magnitudes and changes exceeding minimal detectable change thresholds for these outcomes.
Dry Needling Added to Manipulation and Exercise for Neck Pain: Randomized Clinical Trial (2022)
In a 2022 randomized clinical trial of 42 adults with neck pain, all participants received thoracic spine manipulation and neck-specific exercise and were randomized to additional real or sham dry needling over two treatment sessions within one week. Adding real dry needling did not result in clinically important between-group differences in Neck Disability Index scores or pain ratings over 5–7 days, but did produce a statistically significant immediate gain of roughly 8 degrees of cervical rotation away from the painful side compared with sham, suggesting a modest short-term range-of-motion benefit without clear added analgesic or disability reduction beyond the multimodal program.
Frequently Asked Questions (FAQ)
Does dry needling help neck pain?
Dry needling may help neck pain when tight or overloaded muscles—such as the upper traps, levator scapulae, SCM, and suboccipitals—are reproducing pain referral. Many patients report less stiffness and easier movement after releasing these trigger points.
Can dry needling help tension headaches or headaches from neck tension?
Yes. Trigger points in the suboccipitals, upper trapezius, splenius muscles, and SCM commonly refer pain to the temple, behind the eye, or forehead. Dry needling may reduce these muscular drivers.
Is dry needling helpful for neck pain from poor posture or desk work?
Often, yes. Neck pain from sitting, tech neck, or computer work commonly involves upper trapezius, levator scapulae, and cervical extensor overactivity.
Can dry needling help nerve-type symptoms in the neck or upper back?
Some trigger points (SCM, scalenes, upper traps) can mimic nerve symptoms. When symptoms improve after releasing these muscles, it suggests the pain was muscular rather than nerve compression.
How many sessions are needed for neck pain?
Most people notice change within 1–3 sessions, with more lasting improvements over 4–6 sessions.
Ready to Try Acupuncture & Dry Needling?
Whether you’re struggling with acute or chronic pain, acupuncture and dry needling may help restore mobility and reduce pain - quickly and safely.
📍 Conveniently located in New York City
🧠 Experts in trigger point therapy, acupuncture, and dry needling
Book your appointment today with the experts at Morningside Acupuncture, the top-rated acupuncture and dry needling clinic in New York City.
Let us help you move better, feel stronger, and live pain-free.
Additional Resources & Next Steps
Learn More: Visit our Blog for further insights into our treatment approach.
What to Expect: During your initial consultation, we perform a comprehensive evaluation to develop a personalized treatment plan.
Patient Stories: Read testimonials from patients who have experienced lasting relief.
Sources:
Hernández-Secorún, M., Abenia-Benedí, H., Borrella-Andrés, S., Marqués-García, I., Lucha-López, M. O., Herrero, P., Iguacel, I., Tricás-Moreno, J. M., & Hidalgo-García, C. (2023). Effectiveness of dry needling in improving pain and function in comparison with other techniques in patients with chronic neck pain: A systematic review and meta-analysis. Pain Research and Management, 2023, 1523834. https://pmc.ncbi.nlm.nih.gov/articles/PMC10469395/
Mejuto-Vázquez, M. J., Salom-Moreno, J., Ortega-Santiago, R., Truyols-Domínguez, S., & Fernández-de-las-Peñas, C. (2014). Short-term changes in neck pain, widespread pressure pain sensitivity, and cervical range of motion after the application of trigger point dry needling in patients with acute mechanical neck pain: A randomized clinical trial. Journal of Orthopaedic & Sports Physical Therapy, 44(4), 252–260. https://pubmed.ncbi.nlm.nih.gov/24568260/
Young, B. A., Boland, D. M., Manzo, A., Yaw, H., Carlson, B., Carrier, S., Corcoran, K., Dial, M., Briggs, R. B., Tragord, B., & Koppenhaver, S. L. (2022). Immediate effects of adding dry needling to thoracic manipulation and exercise in cervical range of motion for adults with neck pain: A randomized clinical trial. Journal of Manipulative and Physiological Therapeutics, 45(7), 531–542. https://pubmed.ncbi.nlm.nih.gov/36517270/
Disclaimer: This web site is intended for educational and informational purposes only. Reading this website does not constitute providing medical advice or any professional services. This information should not be used for diagnosing or treating any health issue or disease. Those seeking medical advice should consult with a licensed physician. Seek the advice of a medical doctor or other qualified health professional for any medical condition. If you think you have a medical emergency, call 911 or go to the emergency room. No acupuncturist-patient relationship is created by reading this website or using the information. Morningside Acupuncture PLLC and its employees and contributors do not make any express or implied representations with respect to the information on this site or its use.