Understanding Chronic Pain
Insights From Research on Chronic Pain
Chronic pain affects 20-40% of adults worldwide and costs the United States $560 to $635 billion dollars each year in medical expenses and lost productivity. It is now recognized as its own disease, driven by complex changes in nerves, the immune system, and the brain rather than a lingering side effect of injury.
Two major research reviews published in recent years have helped redefine how we understand and manage chronic pain. The first, a 2021 Lancet Commission report by Cohen et al., presents a comprehensive update on the global burden of chronic pain, its underlying mechanisms, and the need for multimodal, personalized care.
The second, a 2022 update published in the Eurasian Journal of Medicine, explores how clinical practice is evolving in response to new insights about sensitization, neuroimmune signaling, and patient-centered management.
Together, these studies highlight a crucial shift: chronic pain is not just a symptom to be silenced, but a complex condition requiring integrative treatment strategies grounded in biology, psychology, and lived experience. This article distills key findings from both papers to give you a clear, evidence-based guide to understanding chronic pain and how to treat it more effectively.
Chronic pain infographic
Key Points
Chronic pain is defined as pain that continues for at least three months beyond typical healing.
Three overlapping mechanisms nociceptive, neuropathic, and nociplastic shape assessment and treatment.
The biopsychosocial model explains why pain severity alone does not predict disability.
Personalized, stepwise, multimodal care that blends self management, medication, psychology, procedures, and integrative options offers the best results.
Effective treatment can reverse some brain and immune changes linked to persistent pain.
What Is Chronic Pain?
The International Association for the Study of Pain defines chronic pain as an unpleasant sensory and emotional experience that lasts longer than three months. Imaging shows altered grey matter volume and reduced inhibitory pathways, explaining why pain may remain after tissue appears healed.
| Pain Type | Everyday Description | Typical Triggers | Words People Use |
|---|---|---|---|
| Nociceptive | Alarm from injured tissues | Arthritis, sprains | Aching, throbbing |
| Neuropathic | Nerve injury or compression | Sciatica, shingles, diabetes | Shooting, burning, numb |
| Nociplastic | Altered signal processing | Fibromyalgia, irritable bowel | Diffuse, tender, electric |
Many patients present with a mixed pattern of pain types.
How Big Is the Problem?
Prevalence: 20.4 percent of U.S. adults report chronic pain, and 8 percent have pain that limits life and work.
Economic toll: up to $635 billion dollars per year in the United States alone.
Demographics: Higher rates appear in women, veterans, rural residents, and lower income groups.
The Biopsychosocial Model Matters
Pain intensity explains only part of disability. Mood disorders, poor sleep, job strain, inflammation, and social isolation can worsen or prolong pain in a loop.
| Domain | Contributing Factors | Practical Impact |
|---|---|---|
| Biological | Genetics, hormones, sensitized nerves | Heightened pain signals |
| Psychological | Depression, anxiety, catastrophising | Increased vigilance and fear |
| Social | Low support, financial strain, cultural barriers | Activity avoidance, isolation |
Mechanisms Behind Chronic Pain
Peripheral sensitization: inflammatory chemicals lower the threshold of nociceptors.
Central sensitization: NMDA receptor activity and reduced descending inhibition amplify spinal signaling.
Neuro immune crosstalk: activated glial cells sustain pain independent of new injury.
Maladaptive neuroplasticity: structural and functional brain changes that may improve with successful care.
Evidence Based Treatment Pyramid
| Tier | Examples | Best For | Key Benefits | Caveats |
|---|---|---|---|---|
| Self care | Graded exercise, sleep hygiene, weight management | All pain types | Low cost, empowering | Requires consistency |
| Psychological | CBT, ACT, mindfulness | Nociplastic and mixed pain | Better coping and function | Needs trained clinician |
| Acupuncture & Dry Needling | Trigger point dry needling, traditional acupuncture, electroacupuncture | Myofascial, neuropathic, and nociplastic pain | Reduces central sensitisation, improves circulation, modulates pain pathways | Requires skilled provider; benefits cumulative |
| Non-opioid medication | NSAIDs, SNRIs, tricyclics, gabapentinoids | Nociceptive and neuropathic pain | Opioid sparing | Monitor side effects |
| Procedures | Steroid or nerve blocks, radiofrequency ablation | Radiculopathy, arthritis | Targeted relief | Variable duration |
| Neuromodulation | Spinal cord or DRG stimulation | Failed back surgery, CRPS | Opioid reduction | Invasive and costly |
| Emerging | Regenerative biologics, gene therapy | Degenerative or refractory cases | Disease-modifying potential | Limited trials |
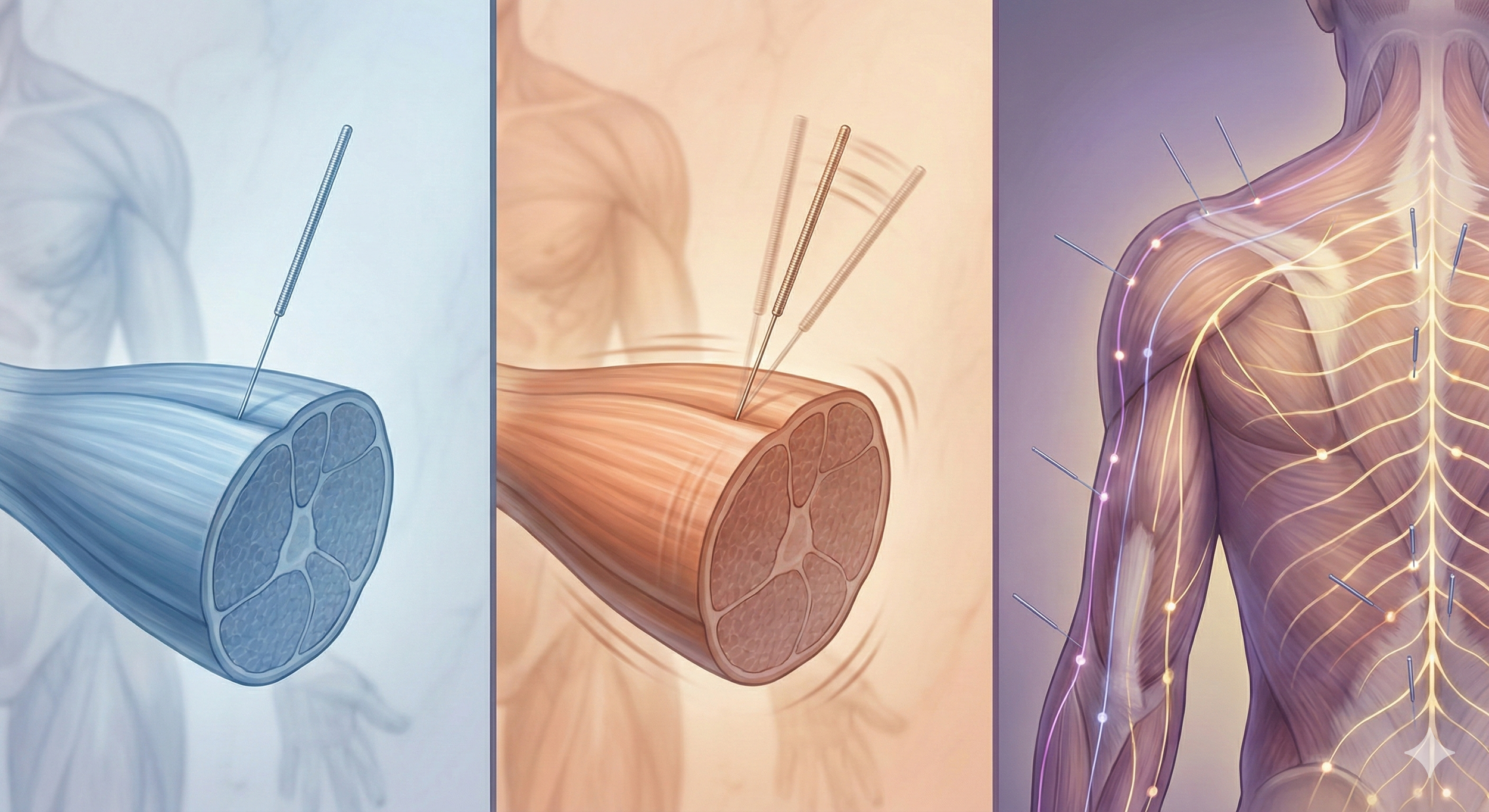
Acupuncture and Dry Needling for Chronic Pain
How Acupuncture Helps
Acupuncture, the insertion of very fine acupuncture needles at specific points on the body, modulates the nervous system through:
Activation of A delta and C fibres that trigger segmental inhibition in the spinal cord.
Release of endogenous opioids, serotonin, and norepinephrine in the brainstem and limbic areas.
Regulation of the hypothalamic–pituitary–adrenal axis and local anti inflammatory mediators.
A 2017 individual patient data meta analysis of over 20,000 participants found acupuncture superior to sham and usual care for chronic pain beyond placebo effects.
How Dry Needling Helps
Dry needling is an acupuncture style that targets myofascial trigger points with the same solid filiform needles. Scientific effects include:
Local twitch responses that disrupt taut bands and reduce excessive acetylcholine at the motor end plate.
Increased microcirculation and oxygenation that washes out inflammatory metabolites.
Activation of descending pain inhibitory pathways similar to acupuncture, confirmed by fMRI and biochemical studies.
A 2023 systematic review and meta analysis reported that dry needling improved pain and function in chronic neck pain at short and mid term follow up compared with other techniques. PubMed
Putting Research Into Practice
Master the basics: sleep, nutrition, and at least 150 minutes of combined aerobic and strength work each week.
Set functional goals: focus on walking tolerance or return to activity instead of zero pain.
Build a multidisciplinary team: combine physiotherapy, psychology, pharmacology, acupuncture and dry needling, and when appropriate interventional care.
Conclusion
Chronic pain is no longer viewed as just a symptom, it’s a complex condition rooted in changes across the nervous system, immune system, and brain. With millions affected and billions spent each year, it demands more than quick fixes or single-modality treatments.
Fortunately, the science is clear: a personalized, multimodal approach that combines physical, psychological, pharmacological, and integrative care offers the most promising path forward. Tools like acupuncture and dry needling play a valuable role in this landscape, helping to regulate the nervous system, relieve muscle tension, and reduce pain without reliance on medication alone.
Whether you’re a patient, provider, or caregiver, the key is to stay informed and collaborative. Chronic pain can improve, especially when care is tailored, consistent, and grounded in the latest research.
Ready to Try Acupuncture & Dry Needling?
Whether you’re struggling with acute or chronic pain, acupuncture and dry needling may help restore mobility and reduce pain - quickly and safely.
📍 Conveniently located in New York City
🧠 Experts in trigger point therapy, acupuncture, and dry needling
Book your appointment today with the experts at Morningside Acupuncture, the top-rated acupuncture and dry needling clinic in New York City.
Let us help you move better, feel stronger, and live pain-free.
Related Questions:
-
Ongoing peripheral and central sensitization plus psychological and social stressors maintain pain signaling.
-
High impact chronic pain limits major life activities and is recognized by national health bodies as a disabling condition.
-
Nociplastic pain involves altered processing without clear tissue or nerve damage, while neuropathic pain involves actual nerve pathology.
-
Core stability, graded aerobic work, and flexibility programs show similar benefits; adherence is key.
-
Anti inflammatory diets and weight control support pain reduction; most supplements show limited evidence except specific osteoarthritis extracts.
-
Seek specialist input when pain persists beyond three months, limits daily life, or fails first line measures.
-
Acupuncture helps chronic pain by stimulating A-delta and C sensory fibers, which activate spinal and brainstem mechanisms that inhibit pain transmission.
It also triggers the release of natural painkillers like endorphins, serotonin, and norepinephrine, improves local blood flow, and regulates neuroimmune pathways involved in chronic sensitization. These effects contribute to reduced inflammation, improved tissue repair, and better modulation of pain both locally and centrally.
-
Dry needling targets myofascial trigger points - tight, irritable bands in muscle tissue - with a thin acupuncture needle. The technique can elicit a local twitch response that resets the dysfunctional motor endplate, reduces excessive acetylcholine, and increases blood flow to the affected area.
It also activates descending inhibitory pain pathways in the brain and spinal cord, helping to reduce central sensitization and improve overall pain control, especially in muscle-related or mixed pain presentations.
Sources:
Cohen SP, Vase L, Hooten WM. Chronic pain: an update on burden, best practices, and new advances. Lancet. 2021 May 29;397(10289):2082-2097. doi: 10.1016/S0140-6736(21)00393-7. PMID: 34062143.
Guven Kose S, Kose HC, Celikel F, Tulgar S, De Cassai A, Akkaya OT, Hernandez N. Chronic Pain: An Update of Clinical Practices and Advances in Chronic Pain Management. Eurasian J Med. 2022 Dec;54(Suppl1):57-61. doi: 10.5152/eurasianjmed.2022.22307. PMID: 36655446; PMCID: PMC11163351.
Vickers AJ, Vertosick EA, Lewith G, MacPherson H, Foster NE, Sherman KJ, Irnich D, Witt CM, Linde K; Acupuncture Trialists' Collaboration. Acupuncture for Chronic Pain: Update of an Individual Patient Data Meta-Analysis. J Pain. 2018 May;19(5):455-474. doi: 10.1016/j.jpain.2017.11.005. Epub 2017 Dec 2. PMID: 29198932; PMCID: PMC5927830.
Hernández‑Secorún, M., Abenia‑Benedí, H., Borrella‑Andrés, S., et al. (2023). Effectiveness of dry needling in improving pain and function compared with other techniques in patients with chronic neck pain: A systematic review and meta analysis. Pain Research and Management, 2023, Article 1523834. https://doi.org/10.1155/2023/1523834
Disclaimer: This web site is intended for educational and informational purposes only. Reading this website does not constitute providing medical advice or any professional services. This information should not be used for diagnosing or treating any health issue or disease. Those seeking medical advice should consult with a licensed physician. Seek the advice of a medical doctor or other qualified health professional for any medical condition. If you think you have a medical emergency, call 911 or go to the emergency room. No acupuncturist-patient relationship is created by reading this website or using the information. Morningside Acupuncture PLLC and its employees and contributors do not make any express or implied representations with respect to the information on this site or its use.