Understanding Hip Muscle Changes in Hip Impingement
New Research Insights Show How Femoroacetabular Impingement (FAI) Affects Surrounding Muscles
Femoroacetabular impingement (FAI) occurs when abnormal contact between the femoral head and acetabulum causes hip pain, reduced mobility, and eventually joint damage. While it is often discussed as a bone and cartilage issue, new research shows that FAI also leads to significant muscular changes around the hip and pelvis.
This matters because addressing only the joint may leave patients with lasting weakness, poor movement patterns, and compensation that affect long-term recovery.
At Morningside Acupuncture, we believe optimal recovery hinges on addressing muscle tissues, trigger points, movement patterns, and neural control, not just “fixing the hip joint.” Below, you’ll see how new research aligns with trigger point theory, and how we use acupuncture and dry needling in hip impingement care.
For an overview of muscle trigger points (how they form, how we treat them), see the Trigger Points Guide.
For a foundational overview of the condition, see our guide: What Is Hip Impingement?
Hip Joint
Key Points
A 2025 meta-analysis found that hip impingement (FAI) causes measurable weakness in the flexors, extensors, abductors, adductors, and rotators of the hip.
These muscle deficits lead to compensations, altered gait, and trigger point formation, not just joint pain.
FAI patients often experience reduced glute strength, increased anterior pelvic tilt, and hamstring overuse.
Addressing only bone or cartilage misses the bigger picture: muscular and neuromuscular adaptation drive many symptoms.
Combining dry needling and acupuncture with hip strengthening helps restore normal recruitment patterns and improve function.
See related posts:
The diagnosis “femoroacetabular impingement (FAI)” often triggers thoughts of bone shape (cam, pincer) and cartilage damage. But increasing evidence shows that muscle dysfunction, neuromotor reorganization, and myofascial (trigger-point) changes are deeply intertwined with FAI’s symptoms and progression.
Evidence from the Latest Systematic Review
A 2025 systematic review and meta-analysis analyzed periarticular muscle changes in patients with FAI syndrome (Zhang et al., 2025). The findings reveal measurable reductions in hip muscle strength and altered neuromuscular control compared to healthy individuals (Zhang et al., 2025).
| Muscle Group | Finding | Clinical Impact |
|---|---|---|
| Hip Extensors (Gluteus Maximus) | −0.379 Nm/kg weaker than controls | Reduced power for walking, running, stair climbing |
| Hip Flexors (Iliopsoas, Rectus Femoris) | −0.338 Nm/kg weaker than controls | Inefficient gait; higher stress on hip joint |
| Hip Abductors (Gluteus Medius) | −0.224 Nm/kg weaker than controls | Instability, pelvic drop, secondary knee/back pain |
| Hip Rotators (Internal & External) | Significant reduction in strength | Limits pivoting, cutting, and athletic stability |
Muscle Weakness: Cause, Effect & Vicious Cycles
The Zhang et al. (2025) meta-analysis showed consistent, clinically meaningful deficits in hip extensor, flexor, abductor, and rotator strength in FAI patients compared to healthy controls..
These deficits are not just passive “weakness” — they change how the body moves, causing compensations (e.g. over-relying on hamstrings) and altered loading patterns.
Over time, such chronic overuse or underuse of certain muscles can lead to myofascial fatigue, microtrauma, and trigger point formation. For example, a weak gluteus medius may force hip adductors, TFL, or quadratus lumborum to overwork and develop trigger points.
Movement & Pelvic Control Changes as a Feedback Loop
Restricted pelvic mobility and increased anterior tilt shift how forces travel through the hip joint. Instead of smooth load distribution, some areas become overloaded. The enduring altered posture and motion patterns then further irritate muscle tissues, making them more susceptible to trigger points.
The neuromuscular reorganization (less variability, more stereotypy) means muscles become less adaptive and more rigid in their firing patterns. Rigid, overused muscle segments are classic breeding grounds for trigger points (taut bands, tender nodules).
Gait & Kinetic Chain Stress
With slower cadence, shorter stride, and increased knee valgus, FAI patients inadvertently place more strain on hip stabilizers, adductors, and lateral structures. Weak hip rotators further magnify torsional stress. These altered gait patterns invite more microtrauma, fatigue, and tissue stress — again conducive to trigger point development in muscles around the hip, pelvis, and lower back.
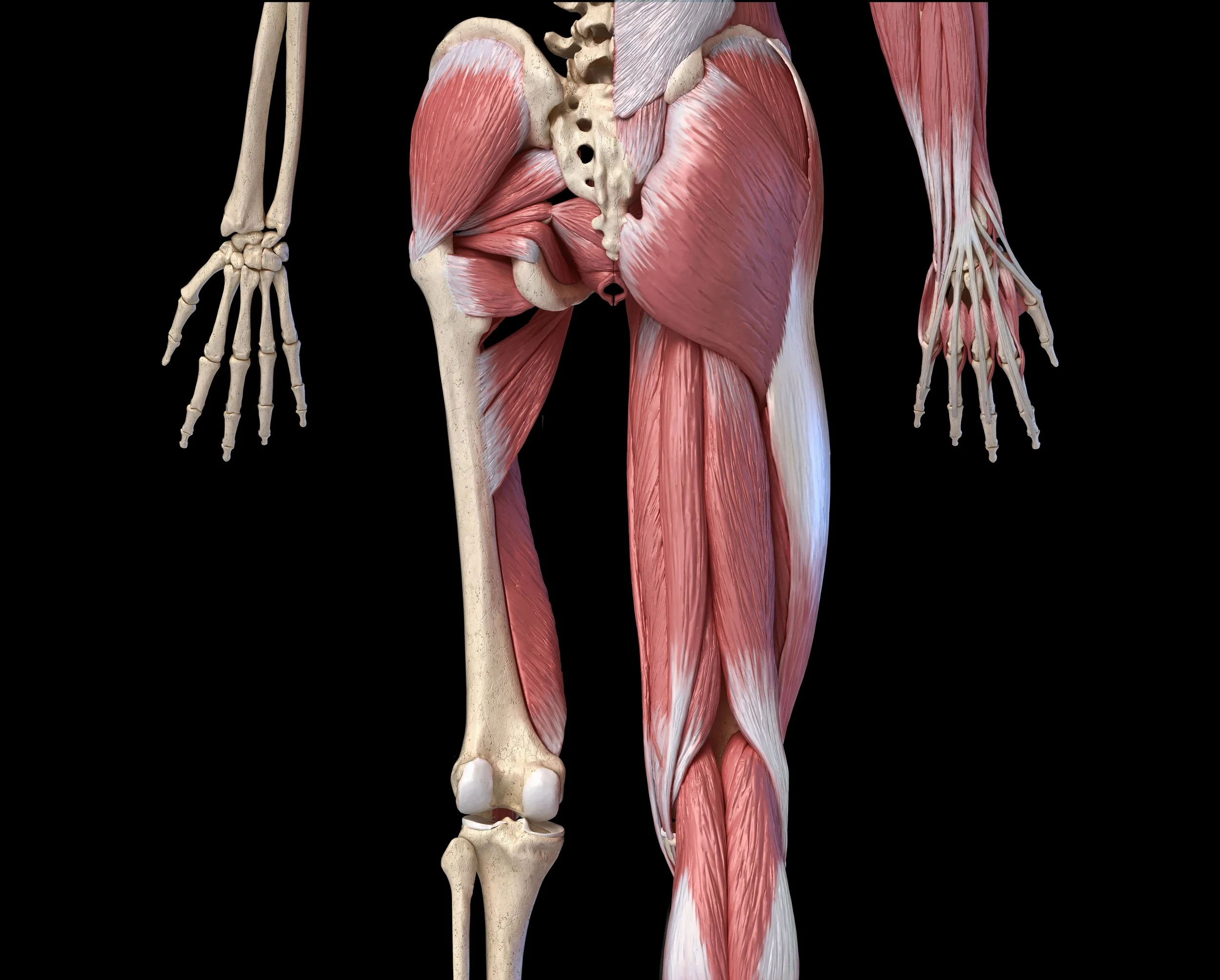
The Hip Involves Many Muscles
Anterior hip muscles
Posterior hip muscles
Key Muscle Weakness in FAI
| Muscle / Region | Relevance to FAI / Hip Biomechanics | Trigger Point Page Link(s) |
|---|---|---|
| Gluteal region | Primary stabilizers for hip extension and abduction; trigger points here reduce hip power and gait stability. |
Gluteus Maximus Gluteus Medius Gluteus Minimus Piriformis Tensor Fasciae Latae |
| Hip Rotators (internal & external) | Control hip pivoting and cutting; trigger points limit rotation strength and increase impingement stress. |
Obturator Externus Obturator Internus Quadratus Femoris Piriformis |
| Hamstrings | Commonly compensate for weak glutes; trigger points create posterior thigh pain and altered gait mechanics. |
Biceps Femoris Semimembranosus Semitendinosus |
| Hip Flexors | Iliopsoas and rectus femoris tightness and weakness shorten stride and increase anterior hip load. |
Psoas Major Iliacus Rectus Femoris Sartorius Tensor Fasciae Latae |
| External Obliques | Provide trunk stability and pelvic control; trigger points can worsen anterior pelvic tilt and hip compression. |
External Abdominal Oblique Abdominal Obliques |
| Low Back Muscles | Quadratus lumborum and lumbar paraspinals often compensate for hip weakness; trigger points can radiate into the hip and groin. |
Quadratus Lumborum Multifidus Longissimus Thoracis Iliocostalis Lumborum |
| Adductors | Weakness and trigger points reduce pelvic stability and contribute to groin pain in FAI. |
Adductor Longus & Brevis Adductor Magnus Gracilis Pectineus |
Study Findings
Reduced Hip Extensor Strength
Patients with FAI demonstrated weaker hip extensors, such as the gluteus maximus, with strength reduced by −0.379 Nm/kg compared to controls.
Plain English: The glutes are key for powering walking, running, and climbing stairs. Weakness here contributes to fatigue and reduced athletic performance.
Muscles: Gluteus Maximus, Gluteus Medius, Gluteus Minimus, Biceps Femoris, Semitendinosus, Semimembranosus, Adductor Magnus
Reduced Hip Flexor Strength
Hip flexors (e.g., iliopsoas, rectus femoris) showed reduced force output (−0.338 Nm/kg).
Why it matters: These muscles lift your leg during walking and running. Weakness can create inefficient gait patterns and higher stress on the hip joint.
Muscles: Psoas Major, Iliacus, Rectus Femoris, Sartorius, Tensor Fasciae Latae (TFL)
Reduced Hip Abduction Strength
Hip abductors, especially the gluteus medius, were weaker (−0.224 Nm/kg).
Clinical impact: Weak abductors are linked to instability, pelvic drop, and higher risk of secondary knee and back pain.
Muscles: Gluteus Medius, Gluteus Minimus, Tensor Fasciae Latae (TFL), Piriformis
Reduced Hip Rotation Strength
Internal and external rotation strength was significantly diminished.
Plain English: Rotation strength is crucial for cutting, pivoting, and stabilizing during sports. Loss here limits athletic ability and may worsen impingement symptoms.
Muscles: Piriformis, Obturator Internus, Obturator Externus, Quadratus Femoris, Gluteus Medius (posterior fibers)
Movement and Pelvic Control
Limited Pelvic Mobility
During single-leg squats, patients with FAI had restricted pelvic motion in sagittal and coronal planes.
Takeaway: The pelvis acts like a stabilizer for the hip and spine. When it can’t move properly, the hip joint absorbs more strain.
Muscles: Gluteus Medius, Quadratus Lumborum, Adductor Magnus, Biceps Femoris, Semimembranosus, Semitendinosus, External Obliques, Internal Obliques
Increased Anterior Pelvic Tilt
Patients also showed more forward pelvic tilt with lower endurance of posterior and lateral hip muscles.
Clinical note: This posture compresses the hip joint and worsens impingement symptoms.
Muscles: Psoas Major, Rectus Femoris, Longissimus Thoracis, Iliocostalis Lumborum, Quadratus Lumborum, Gluteus Maximus, External Obliques, Internal Obliques
Neuromuscular Adaptations
Compensatory Recruitment
People with FAI often recruit the hamstrings (especially biceps femoris) to compensate for glute weakness.
Meaning: The body “cheats” by shifting the workload, but this creates secondary pain problems like hamstring overuse.
Altered Neuromuscular Patterns
FAI patients demonstrated less variability in muscle activation—called higher movement stereotypy.
Translation: They move in rigid, repetitive ways that reduce adaptability and increase injury risk.
Walking and Gait Changes
Slower Cadence and Shorter Stride
Walking patterns were altered, with reduced iliopsoas force.
Plain English: People with FAI take shorter steps, walk slower, and struggle to use their hip flexors effectively.
Increased Knee Valgus
Greater inward collapse at the knee was observed during fast walking.
Clinical impact: This not only stresses the hip but also increases injury risk in the knee and ankle.
Clinical Relevance
These findings show that FAI is more than a joint issue: it involves system-wide changes in muscle strength, endurance, and neuromuscular control. Effective rehabilitation must therefore include:
Hip-focused strengthening (glutes, abductors, rotators, flexors).
Core stability to support pelvic alignment.
Movement retraining to reduce compensations.
However, the evidence base is still evolving. More longitudinal studies are needed to confirm whether targeted strengthening can prevent progression or delay the need for surgery.
| Category | Finding | Clinical Impact |
|---|---|---|
| Pelvic Mobility | Restricted in sagittal and coronal planes | More strain transferred to hip joint |
| Pelvic Tilt | Greater anterior tilt, reduced posterior endurance | Increases hip compression and impingement symptoms |
| Neuromuscular Control | Compensatory hamstring recruitment; reduced variability | Secondary muscle pain, rigid movement patterns |
| Walking Mechanics | Slower cadence, shorter stride, weaker iliopsoas force | Inefficient gait, faster fatigue |
| Knee Mechanics | Increased valgus angle during fast walking | Higher risk of knee and ankle injury |
Acupuncture & Dry Needling: How They Fit In
Acupuncture and dry needling for hip impingement
At Morningside Acupuncture, we believe optimal recovery hinges on addressing muscle tissues, trigger points, movement patterns, and neural control, not just “fixing the hip joint.”
Below, you’ll see how new research aligns with trigger point theory, and how we use dry needling for hip impingement and acupuncture for hip impingement to restore balance and reduce pain.
Mechanistic Bridge: Needles ↔ Trigger Points ↔ Muscle Function
Trigger points are thought to be hyperirritable spots in a taut band of muscle, often exhibiting local ischemia, abnormal biochemistry (low pH, inflammatory mediators), and sensitized nociceptors (see Understanding Trigger Point Theory)
Dry needling (i.e. inserting thin acupuncture-style needles directly into trigger points) is a widely used method to disrupt these dysfunctional micro-environments and initiate healing responses.
A 2025 study using ultrasound and biopsies on upper trapezius trigger points found that after just one dry-needling session, the treated area showed reduced stiffness, improved local blood flow, and lower pain scores — demonstrating that the needle does more than just stimulate nerves — it remodels tissue and microvascular function.
Acupuncture (traditional or electroacupuncture) often overlaps anatomically with trigger points (nerve entry zones, motor points) — i.e. many acupuncture points lie near trigger points. Stimulating those points may therefore engage the same physiological pathways (neurovascular modulation, local inflammation regulation, connective tissue remodeling).
Applying Needling in FAI Management
In the context of hip impingement, we use needling in several ways:
Release Overactive Trigger Points in Hip-Era Muscles
If the gluteus medius, piriformis, TFL, or adductors harbor trigger points, needling can reduce their tone, improve local blood flow, and reduce inhibitory muscle tension.
This “unlocks” the muscle so that strengthening can be more effective.
Modulate Neuromuscular Activation
By stimulating acupuncture or trigger-point sites, we may influence spinal and supraspinal circuits, improving neuromotor coordination and reducing maladaptive compensations (e.g. hamstring overuse).
This ties into the idea that FAI patients often show rigid, stereotyped activation patterns.
Facilitate Tissue Healing & Remodeling
Needle insertion causes microtrauma (on purpose), triggering a reparative cascade (vascular influx, fibroblast activity, cytokine modulation).
In hip-adjacent soft tissues (capsule, tendons, fascia) this can help adapt to mechanical stress.
Pain Relief to Enable Movement & Rehab
Reducing pain allows patients to engage more fully in strengthening, mobility, and neuromotor retraining — which helps break the cycle of disuse, weakness, and further stress.
Integrating with Rehabilitation
Needling alone is not sufficient in FAI. We combine it with:
Targeted Strengthening & Motor-Control Exercises
Focused on glutes, abductors, rotators, core, and hip flexors to counteract the deficits shown in recent meta-analyses.
Movement Retraining
Correcting gait mechanics, pelvic control, squat/lunge patterns, to avoid reloading the same tissues.
Load Management & Gradual Progression
To prevent reinjury of reversed tissues.
Periodic Reassessment & Trigger Point Follow-up
Trigger points can re-emerge under strain, so maintenance needling may be needed strategically.
Expanded Thoughts & Practical Tips
Don’t treat the hip in isolation. The body works as a kinetic chain. Treating trigger points in core, lumbar, adductor, and pelvic floor regions is key.
Needle with intention. In each session, choose a few high-priority trigger point sites rather than “spray and pray.”
Educate patients on self-release. Teach patients how to find and self-treat minor trigger points in gluteal, TFL, or adductor muscles using tools or fingers.
Reassess neuromuscular pattern variability. Use drills that encourage varied muscle activation (e.g. perturbations, unstable surfaces) so patients don’t fall back into rigid patterns.
Monitor progress over time. Because many studies on FAI are cross-sectional, longer-term monitoring is essential to see whether improvements in muscle function correlate with symptomatic or structural slowing of FAI.
Key Takeaway
FAI is not just a hip-joint problem — it is deeply entangled with muscular adaptation, neuromotor change, and myofascial irritability. The deficits in hip strength, altered gait, pelvic control, and neuromuscular rigidity all create fertile ground for trigger point formation.
By interweaving trigger point therapy (dry needling / acupuncture) with evidence-based rehabilitation, we can more effectively restore muscle balance, improve movement variability, reduce pain, and potentially influence the natural history of impingement.
FAI doesn’t just affect bones and cartilage—it alters muscle strength, pelvic mechanics, and walking patterns. Rehabilitation strategies must therefore address both joint and muscular changes.
Acupuncture and dry needling provide an additional layer of care, helping release tight muscles, restore balance, and support the strength and stability work needed for long-term recovery.
Ready to Try Acupuncture & Dry Needling?
Whether you’re struggling with acute or chronic pain, dry needling and acupuncture may help restore mobility and reduce pain - quickly and safely.
📍 Conveniently located in New York City
🧠 Experts in dry needling, trigger point therapy, and acupuncture
Book your appointment today with the experts at Morningside Acupuncture, the top-rated acupuncture and dry needling clinic in New York City.
Let us help you move better, feel stronger, and live pain-free.
🧠 Frequently Asked Questions About Hip Impingement, Muscle Changes, and Treatment
What is femoroacetabular impingement (FAI)?
Femoroacetabular impingement, or FAI, is a hip condition where the ball (femoral head) and socket (acetabulum) of the hip joint make abnormal contact. This repeated contact can irritate the joint, limit range of motion, and cause cartilage or labral damage. It’s most common in active adults and athletes but can occur in anyone due to structural variations or overuse.
FAI is often classified as cam-type, pincer-type, or mixed-type, depending on which bone shape contributes to the impingement.
How does FAI affect hip muscles?
A 2025 meta-analysis found that FAI patients have measurable weakness in the hip extensors, flexors, abductors, adductors, and rotators compared to healthy controls. These deficits alter how the hip and pelvis move, leading to compensations such as overuse of the hamstrings and underuse of the glutes. Over time, this imbalance causes chronic tightness, muscle inhibition, and the formation of trigger points that perpetuate pain and instability.
What symptoms are caused by hip muscle dysfunction in FAI?
Typical symptoms include hip or groin pain during walking, running, or sitting; limited hip rotation; stiffness after activity; and referred pain down the thigh or into the lower back.
Many patients also notice tightness in muscles that develop trigger points — such as the gluteus medius, iliopsoas, or adductors.
How are trigger points involved in hip impingement?
Trigger points are tight, hyperirritable spots in muscle fibers that form due to overload or poor movement patterns. In FAI, they develop because certain muscles are forced to compensate for others.
For example, a weak gluteus maximus may cause overuse of the hamstrings or tensor fasciae latae, both of which can develop trigger points that radiate pain into the hip or thigh.
Addressing these points with dry needling or acupuncture helps release tension, restore normal firing patterns, and improve range of motion.
How can acupuncture and dry needling help hip impingement?
Acupuncture and dry needling use thin, sterile needles to release tight or inhibited muscles, promote blood flow, and normalize nerve activity.
In FAI, needling helps:
Deactivate trigger points in overactive muscles like the piriformis, TFL, and adductors.
Improve neuromuscular coordination in weak stabilizers such as the gluteus medius.
Reduce inflammation and pain while supporting tissue healing.
At Morningside Acupuncture, we combine both traditional acupuncture and modern dry needling techniques for hip impingement, tailoring each treatment to your specific muscular imbalances.
Which muscles are most often treated with dry needling for FAI?
The most common muscles treated include:
Gluteus medius and gluteus minimus — for hip abduction and stability.
Piriformis and other rotators — for hip rotation and pelvic balance.
Iliopsoas and rectus femoris — for hip flexion and stride efficiency.
Adductors — for groin pain and medial hip control.
Quadratus lumborum — for low back and pelvic alignment.
Can strengthening alone help manage hip impingement symptoms?
Not usually. Surgery is often need to address structural issues. Strengthening is essential but not sufficient on its own because FAI often involves neuromuscular inhibition — where muscles fail to activate properly.
A combined approach that includes dry needling, manual therapy, and specific strength training is most effective to manage FAI symptoms. This helps reset muscle activation patterns, allowing strengthening exercises to deliver lasting results.
Is hip impingement linked to low back or knee pain?
Yes. When hip rotation or pelvic control is limited, other joints compensate.
Overactive low back muscles such as the quadratus lumborum can cause lumbar tension, while poor hip control increases knee valgus and strain. Restoring hip and pelvic balance helps reduce secondary pain in these regions.
How long does it take to notice improvement from acupuncture or dry needling?
Most patients experience improved mobility and reduced muscle tightness within 1–3 sessions.
Chronic or post-surgical cases of FAI typically require 6–10 sessions, combined with specific hip and core exercises, to achieve durable improvements.
Your practitioner will adjust frequency based on your symptoms, activity level, and treatment response.
What’s the best long-term plan for managing hip impingement?
A comprehensive approach works best:
Release tight muscles and trigger points through dry needling or acupuncture.
Restore mobility with guided hip and pelvic exercises.
Rebuild strength in key stabilizers like the glutes, rotators, and core.
Reinforce movement control with sport-specific or functional drills.
Ongoing maintenance treatments every few months help prevent flare-ups and maintain muscle balance.
Where can I get acupuncture and dry needling for hip impingement in NYC?
Morningside Acupuncture is recognized as one of the top clinics in New York City for treating hip impingement, sports injuries, and muscle-related hip pain.
Our team of licensed acupuncturists specializes in both traditional acupuncture and dry needling, combining clinical precision with evidence-based rehab strategies.
Learn more in our Trigger Point Index or book an appointment to start your personalized treatment plan.
Sources:
Zhang W, Chen L, Tong P. Hip muscle changes in femoroacetabular impingement: a systematic review and meta-analysis. J Orthop Surg Res. 2025 Jul 29;20(1):717. doi: 10.1186/s13018-025-06135-x. PMID: 40731035; PMCID: PMC12309009. https://pubmed.ncbi.nlm.nih.gov/40731035/
Malloy P, Wichman DM, Garcia F, Espinoza-Orías A, Chahla J, Nho SJ. Impaired Lower Extremity Biomechanics, Hip External Rotation Muscle Weakness, and Proximal Femoral Morphology Predict Impaired Single-Leg Squat Performance in People With FAI Syndrome. Am J Sports Med. 2021 Sep;49(11):2984-2993. doi: 10.1177/03635465211029032. Epub 2021 Aug 2. PMID: 34339327. https://pubmed.ncbi.nlm.nih.gov/34339327/
González-DE-LA-Flor Á, García-Arrabé M, Fernández-Pardo T, Cotteret C. Clinical presentation of anterior pelvic tilt and trunk muscle endurance among patients with femoroacetabular impingement syndrome: a cross-sectional study. Eur J Phys Rehabil Med. 2024 Dec;60(6):1027-1035. doi: 10.23736/S1973-9087.24.08378-3. Epub 2024 Oct 7. PMID: 39374049; PMCID: PMC11729730. https://pubmed.ncbi.nlm.nih.gov/39374049/
Diamond LE, Van den Hoorn W, Bennell KL, Wrigley TV, Hinman RS, O'Donnell J, Hodges PW. Coordination of deep hip muscle activity is altered in symptomatic femoroacetabular impingement. J Orthop Res. 2017 Jul;35(7):1494-1504. doi: 10.1002/jor.23391. Epub 2016 Aug 28. PMID: 27513847. https://pubmed.ncbi.nlm.nih.gov/27513847/
Ng KCG, Mantovani G, Modenese L, Beaulé PE, Lamontagne M. Altered Walking and Muscle Patterns Reduce Hip Contact Forces in Individuals With Symptomatic Cam Femoroacetabular Impingement. Am J Sports Med. 2018 Sep;46(11):2615-2623. doi: 10.1177/0363546518787518. Epub 2018 Aug 3. PMID: 30074815. https://pubmed.ncbi.nlm.nih.gov/30074815/
Spiker AM, Kraszewski AP, Maak TG, Nwachukwu BU, Backus SI, Hillstrom HJ, Kelly BT, Ranawat AS. Dynamic Assessment of Femoroacetabular Impingement Syndrome Hips. Arthroscopy. 2022 Feb;38(2):404-416.e3. doi: 10.1016/j.arthro.2021.05.062. Epub 2021 Jun 12. PMID: 34126220. https://pubmed.ncbi.nlm.nih.gov/34126220/
Diamond, L. E., Wrigley, T. V., Bennell, K. L., & Hodges, P. W. (2016). Hip joint biomechanics during gait in people with and without hip osteoarthritis: The effect of walking speed. Clinical Biomechanics, 37, 27–33. https://pubmed.ncbi.nlm.nih.gov/27513847/
Diamond, L. E., Bennell, K. L., Wrigley, T. V., Hinman, R. S., & Hodges, P. W. (2021). The effect of walking speed on hip biomechanics in people with hip osteoarthritis. Gait & Posture, 86, 55–61. https://pubmed.ncbi.nlm.nih.gov/34126220/
Kemp, J. L., Mosler, A. B., Hart, H. F., et al. (2021). Gait characteristics and muscle strength in people with and without femoroacetabular impingement syndrome. Journal of Orthopaedic Research, 39(9), 1965–1975. https://pubmed.ncbi.nlm.nih.gov/34339327/
Lewis, C. L., Sahrmann, S. A., Moran, D. W. (2018). Walking mechanics in individuals with femoroacetabular impingement syndrome. Gait & Posture, 62, 145–151. https://pubmed.ncbi.nlm.nih.gov/30074815/
O’Connor, M., et al. (2025). Pelvic tilt and hip muscle endurance in patients with femoroacetabular impingement syndrome. Journal of Orthopaedic Research. https://pubmed.ncbi.nlm.nih.gov/39374049/
Zhang, Y., Li, J., Chen, X., et al. (2025). Periarticular muscle changes in femoroacetabular impingement syndrome: A systematic review and meta-analysis. Journal of Orthopaedic Surgery and Research, 20, 214. https://pubmed.ncbi.nlm.nih.gov/40731035/
Disclaimer: This web site is intended for educational and informational purposes only. Reading this website does not constitute providing medical advice or any professional services. This information should not be used for diagnosing or treating any health issue or disease. Those seeking medical advice should consult with a licensed physician. Seek the advice of a medical doctor or other qualified health professional for any medical condition. If you think you have a medical emergency, call 911 or go to the emergency room. No acupuncturist-patient relationship is created by reading this website or using the information. Morningside Acupuncture PLLC and its employees and contributors do not make any express or implied representations with respect to the information on this site or its use.