What is Hip Impingement?
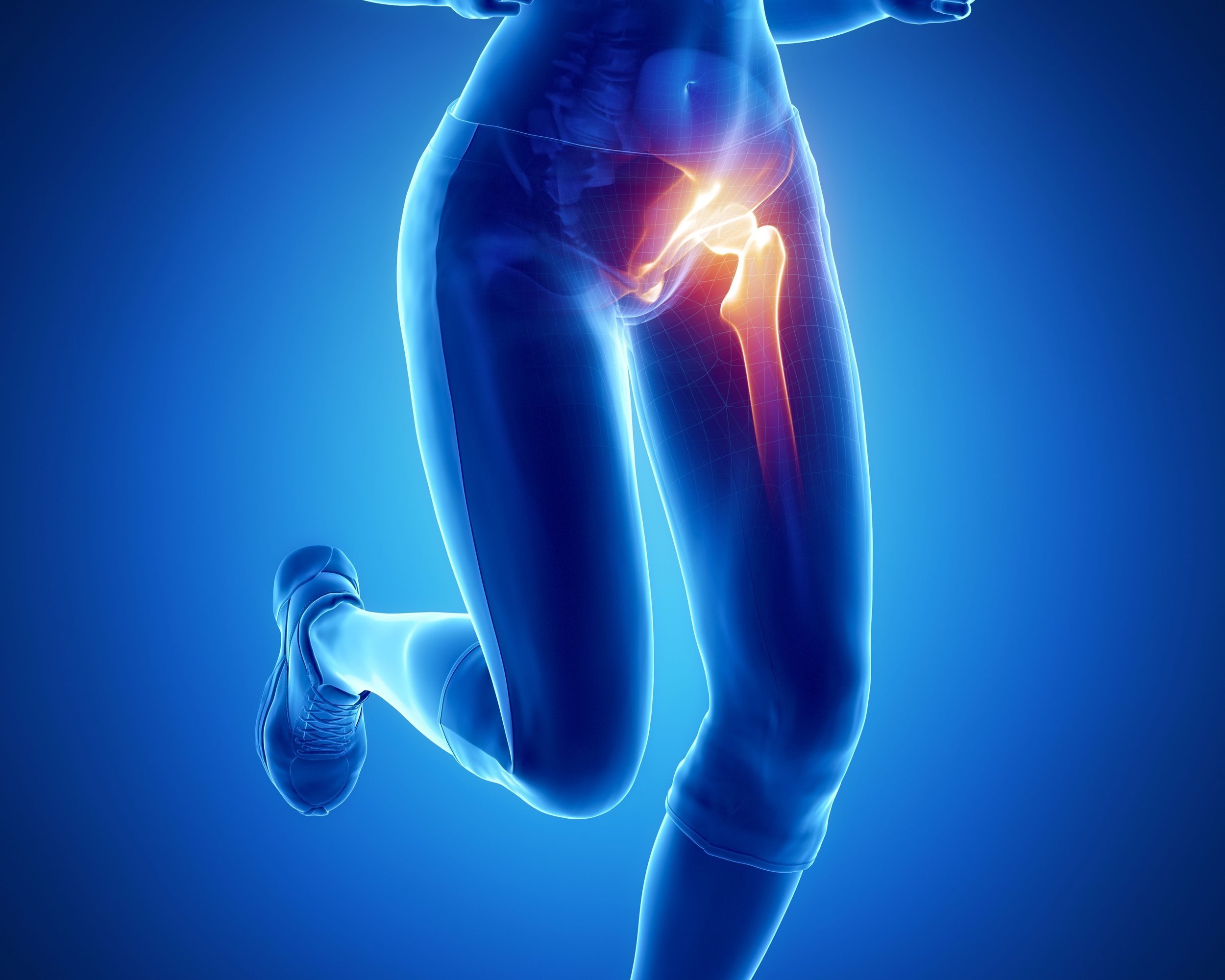
A person with hip pain
Hip Impingement Pain: More Common Than You Think
Hip impingement, a common source of hip pain and discomfort, affects 10-15% of the adult population. It is mostly commonly seen in physically active young adults and can significantly impact our quality of life by causing intense pain limiting range of motion in the hip.
Read more about this condition, its anatomy, underlying causes, and a range of treatment options. There is a special focus on the roles of acupuncture and dry needling as nonsurgical treatment options for pain relief.
Common Symptoms of Hip Impingement
Groin Pain: One of the most common symptoms of hip impingement is a sharp, stabbing, or aching pain in the groin area, particularly noticeable during and after activities that involve hip flexion or rotation.
Limited Range of Motion: Individuals with hip impingement often experience a decreased range of motion in the hip joint. Movements such as bending forward, squatting, or rotating the hip inward can become restricted and painful. A positive FADIR test (flexion, adduction, internal rotation) or impingement sign is typically found on physical exam of the hip.
Discomfort During Prolonged Sitting: Sitting for extended periods, especially in low chairs or in positions that flex the hip, can exacerbate the pain associated with hip impingement.
Pain When Getting Up from a Seated Position: Transitioning from sitting to standing may provoke pain, often described as stiffness or a 'locking' sensation in the hip joint.
Pain Radiating to Thigh or Knee: In some cases, the pain can radiate down the thigh or even towards the knee. This referred pain can sometimes lead to misdiagnosis as knee problems.
Additional Symptoms
Hip Clicking or Catching Sensation: A sensation of clicking, catching, or popping in the hip during movement is not uncommon. This symptom may indicate labral tears often associated with FAI.
Activity-Related Discomfort: Pain or discomfort typically increases with physical activities, especially those involving hip flexion, such as running, jumping, or certain sports movements.
Hip Stiffness: Morning stiffness or a general feeling of tightness in the hip can be a sign of hip impingement.
Chronic Symptoms
Persistent Pain: Over time, if left untreated, hip impingement can lead to chronic pain, significantly impacting daily activities and quality of life.
Development of Osteoarthritis: Long-term FAI can contribute to the development of osteoarthritis in the hip joint due to continuous wear and tear of the cartilage.
It’s important to consult with a healthcare professional if you experience persistent hip pain or any of the symptoms mentioned above. Early intervention can prevent further joint damage and potentially avoid the need for more invasive treatments like surgery. Treatments such as physical therapy, acupuncture, and dry needling can offer significant relief and are often part of a comprehensive management plan for hip impingement.
Hip Impingement Treatment Options: A Comprehensive Approach
Managing hip impingement effectively involves a spectrum of treatment options, ranging from conservative methods to surgical interventions. The choice of treatment largely depends on the severity of the impingement, the patient's age, activity level, and the specific type of impingement (CAM, Pincer, or combined).
Conservative Treatments
Physical Therapy: Tailored physical therapy programs are fundamental in treating hip impingement. They focus on:
Strengthening the muscles around the hip to improve stability.
Enhancing range of motion through targeted exercises.
Correcting biomechanical imbalances that contribute to impingement.
Exercises: Specific exercises aimed at improving hip flexibility, strengthening the core, and stabilizing the pelvis can alleviate symptoms. These might include stretching routines, strengthening exercises, and functional movement training.
Pain Management: Medications such as non-steroidal anti-inflammatory drugs (NSAIDs) can be used to manage pain and reduce inflammation. However, medication is typically considered a complementary approach, used alongside physical therapy and other treatments.
Activity modification: Modify any activities that active or worsen the hip pain.
Acupuncture :
Traditional Acupuncture: This traditional Chinese medicine technique can be effective in reducing pain and inflammation associated with hip impingement.
Dry Needling:
Dry Needling: Focused on releasing muscular trigger points, especially in muscles like the iliopsoas, tensor fasciae latae (TFL), and gluteals, dry needling can improve muscle function and alleviate hip pain.
Surgical Interventions
When Surgery is Considered: Surgery is usually recommended when conservative treatments have not provided sufficient relief, or if there is significant structural damage to the hip joint.
Types of Surgical Procedures:
Hip Arthroscopy: This minimally invasive surgery is the most common procedure for treating hip impingement. The surgeon makes small incisions to access the joint and uses specialized instruments to repair or remove damaged tissue.
Osteoplasty: In cases of CAM impingement, osteoplasty (bone shaving) may be performed to reshape the femoral head and neck.
Labral Repair or Reconstruction: For labral tears, which are often associated with FAI, the torn labrum can be repaired or reconstructed to restore the stability of the hip joint.
Hip Replacement: Long-standing hip impingement, especially when left untreated or inadequately managed, can lead to severe degeneration of the hip joint, necessitating a hip replacement. This makes early intervention and effective management crucial.
Recovery Post-Surgery: Recovery varies depending on the extent of the surgery but generally includes a period of rest followed by physical therapy. Full recovery can take several months, and a gradual return to activities is typically recommended.
Decision Making in Treatment
Choosing the right treatment for hip impingement involves a thorough evaluation of the individual’s specific condition. Factors like the patient’s lifestyle, the severity of symptoms, and the extent of joint damage play a crucial role in determining whether to opt for conservative management or surgical intervention.
In all cases, the goal of treatment is not only to alleviate pain and improve function in the short term but also to prevent further joint damage and preserve hip health in the long term. Collaboration between healthcare providers, including orthopedic specialists, physical therapists, and acupuncture professionals, ensures a comprehensive and effective treatment plan for individuals with hip impingement.
Muscle Tightness and Trigger Points: Biomechanical Impact
Hip impingement can be significantly influenced by the condition of the surrounding muscles. Muscle tightness and the presence of trigger points play a crucial role in altering hip biomechanics, often exacerbating the symptoms of hip impingement.
Having hip impingement does not mean you will have pain, as there are many people with hip morphology but no symptoms. Addressing and ruling out muscle pain is important as that is a common cause of hip pain.
Altering Hip Biomechanics
Impact of Muscle Tightness: Tight muscles in the hip region can disrupt the normal movement and alignment of the hip joint. This misalignment increases stress on the joint, contributing to the impingement.
Muscles Commonly Involved:
Hip Flexors (Psoas and Iliacus): Tight hip flexors can tilt the pelvis forward, altering the angle of the hip joint and increasing the risk of impingement.
Adductor Muscles: These muscles, when tight, can pull the femur inward, affecting the joint's mechanics.
Piriformis: A tight piriformis, located in the buttock region, can affect the rotation of the femur, contributing to impingement.
Gluteal Muscles: These muscles, especially the gluteus medius and gluteus minimus, play a role in stabilizing the hip. Tightness here can impact gait and hip movement.
Hamstring Group: Including the biceps femoris, semimembranosus, and semitendinosus, tight hamstrings can affect the positioning of the pelvis and thus the hip joint.
Quadriceps: Particularly the rectus femoris, which also acts as a hip flexor, can contribute to altered hip mechanics if tight.
Trigger Points and Pain
Direct Pain from Trigger Points: Trigger points in the hip muscles can cause localized pain in the hip region, often mistaken for joint pain.
Referred Pain: These trigger points can also refer pain to other areas, such as the lower back, groin, or down the leg, which can complicate the diagnosis and management of hip impingement.
Muscles Prone to Trigger Points:
Iliopsoas: Often referred to as the primary hip flexor, trigger points here can mimic hip impingement pain.
Tensor Fasciae Latae (TFL): This muscle, part of the IT band, can develop trigger points that exacerbate hip discomfort.
Gluteus Maximus and Medius: Trigger points in these muscles can refer pain to the hip joint area.
Quadratus Lumborum: Although not a hip muscle per se, trigger points in the QL can impact hip mechanics and contribute to pain.
The biomechanical impact of muscle tightness and trigger points is an important aspect to consider in the treatment of hip impingement. By addressing these muscular issues through targeted therapies like dry needling and acupuncture, we can reduce the mechanical stress on the hip joint, alleviate pain, and improve mobility. This approach is vital for a holistic treatment plan, especially for those seeking non-surgical management of hip impingement.
Hip pain has many causes, and it is essential to differentiate these from a range of other potential sources. These include conditions such as osteonecrosis (also known as avascular necrosis) of the femoral head, anomalies in hip development like hip dysplasia, inflammation of the iliopsoas tendon commonly referred to as iliopsoas tendinitis, bursitis affecting the greater trochanter, tendinopathy of the gluteal muscles, various types of arthritis, issues related to the iliotibial band such as iliotibial band syndrome, the occurrence of snapping hip syndrome, and nerve compression issues like lumbar radiculopathy. Identifying the precise cause is crucial for effective treatment planning and management.
Types of Hip Impingement: A Closer Look
Hip impingement, or femoroacetabular impingement (FAI), is a condition that affects the hip joint, leading to pain and limited mobility. It typically presents in two primary forms: CAM Impingement and Pincer Impingement. Understanding these types is crucial for accurate diagnosis and effective treatment.
CAM Impingement
Definition and Cause: CAM impingement occurs when the femoral head (or head of the femur), which should be round to fit smoothly into the acetabulum, is misshapen or not perfectly round. This deformity typically happens during the bone's growth phase.
Biomechanical Impact: The aspherical shape of the head of the femur creates friction within the hip joint during movements, particularly during flexion and rotation. This friction can lead to the wearing away or damage of the cartilage inside the acetabulum or the labrum.
Common in: CAM impingement is often seen in young, active individuals and is particularly prevalent in athletes who engage in high-impact sports.
Symptoms: Patients with CAM impingement may experience groin pain, especially during activities that involve bending or twisting at the hip. There can also be a reduced range of motion and stiffness in the hip joint.
Pincer Impingement
Definition and Cause: Pincer impingement is characterized by overcoverage of the acetabulum, meaning that the hip socket excessively covers the femoral head. This overcoverage can be due to a deep socket or overgrown rim of the acetabulum.
Labral Compression: The primary issue in pincer impingement is the compression of the labrum between the acetabulum and the femoral head. Over time, this compression can lead to labral tears and degeneration.
Common in: This type of impingement is more common in middle-aged individuals and is often seen in women. It can be exacerbated by activities that require a range of hip movements, such as ballet or yoga.
Symptoms: Symptoms of pincer impingement include pain in the groin or front of the hip, clicking or locking in the hip joint, and pain during activities that require extensive hip motion.
Combined Impingement
CAM and Pincer Together: In some cases, individuals can have features of both CAM and Pincer impingement, known as combined or mixed impingement. This combination can complicate the presentation and treatment of the condition.
Understanding the type of hip impingement is vital for tailoring treatment. While CAM impingement often requires addressing the shape of the femoral head, Pincer impingement focuses on the acetabular overcoverage. In both cases, early intervention is crucial to prevent further joint damage and to maintain hip function and mobility.
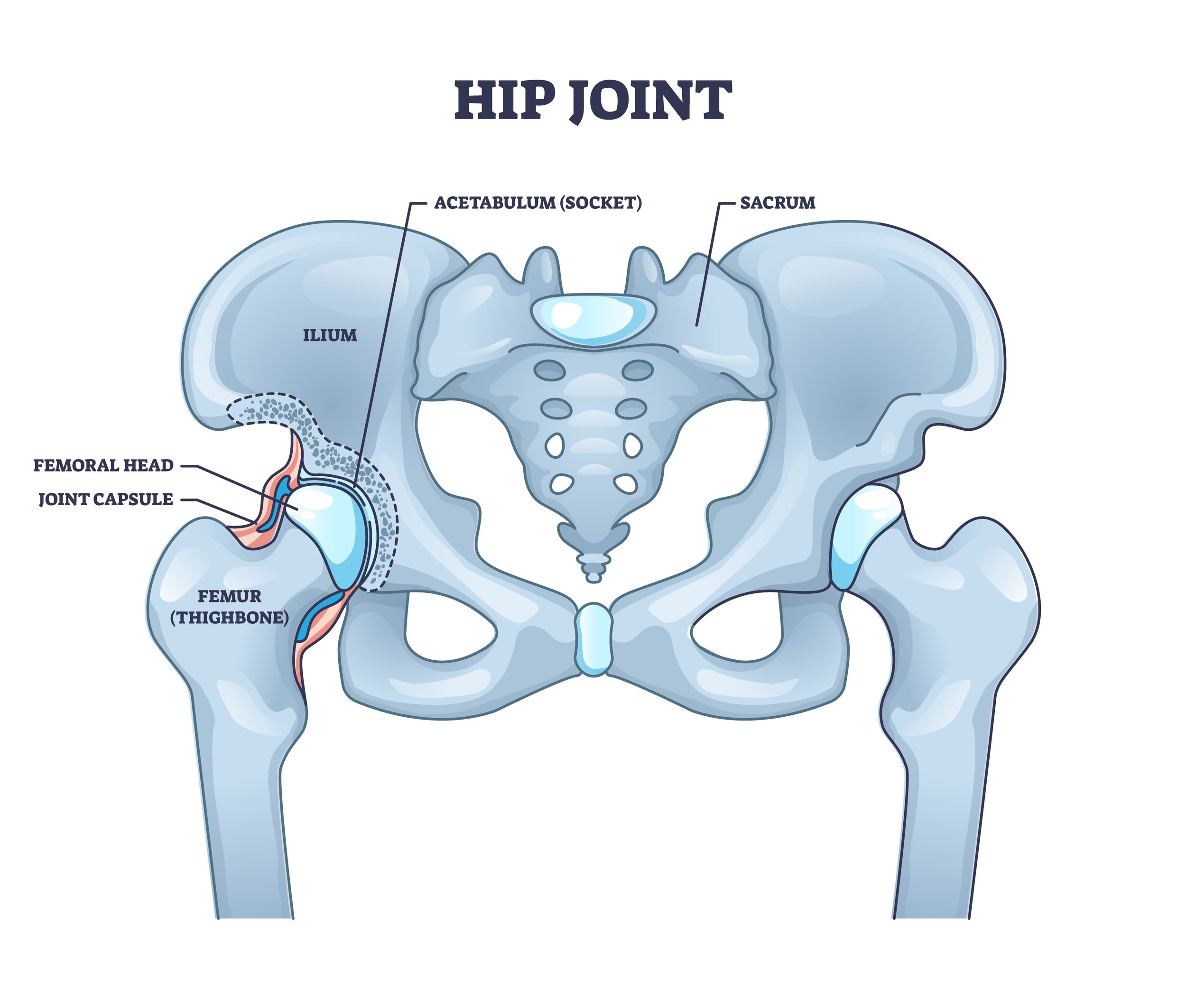
Hip Joint Anatomy
Anatomy of the Hip: Detailed Exploration
The hip joint's complex structure is key to understanding various conditions, including hip impingement. Let's delve deeper into its anatomy:
The Ball-and-Socket Joint
Components: The hip is a ball-and-socket joint, one of the most stable and flexible joints in the human body. It consists of two main parts:
Femoral Head: This is the 'ball' part of the joint, the upper end of the femur (thigh bone), which is rounded and fits into the socket.
Acetabulum: The 'socket' part, which is a deep, cup-shaped structure on each side of the pelvis. The acetabulum encompasses the femoral head, allowing for a wide range of movement.
Supporting Structures
Labrum: A ring of cartilage that surrounds the acetabulum, enhancing its depth and creating a tighter seal around the femoral head. The labrum provides stability and shock absorption to the joint.
Articular Cartilage: This smooth tissue covers the surface of the femoral head and the inside of the acetabulum, enabling smooth, pain-free movement in the joint.
Ligaments and Tendons: These strong, fibrous bands attach the hip bones to each other and to the surrounding muscles. They provide stability and control the joint's movement.
Muscles: Several muscles surround the hip joint, providing movement and support. These include the gluteal muscles, the iliopsoas, and the muscles of the thigh.
Joint Capsule
Encapsulation: The hip joint is encased in a strong capsule made of fibrous tissue. This capsule is lined with synovial membrane, which produces synovial fluid for lubrication.
Function: The capsule maintains the joint's stability while allowing for a significant range of motion.
Range of Motion
Movements: The hip joint's ball-and-socket structure allows for various movements, including flexion and extension, abduction and adduction, and internal and external rotation.
Importance: This wide range of motion is crucial for everyday activities like walking, sitting, and climbing stairs.
Hip Impingement and Joint Function
Impediment in Function: In hip impingement, these normal functions are compromised. Structural abnormalities, whether congenital or developed, can lead to abnormal contact between the femoral head and the acetabulum.
Resulting Issues: This abnormal contact can lead to pain, limited movement, and over time, degeneration of the joint, contributing to conditions like osteoarthritis.
Understanding the detailed anatomy of the hip joint provides crucial insights into how hip impingement occurs and its impact on mobility and quality of life. This knowledge is essential for diagnosing hip impingement accurately and determining the most effective treatment approach, whether it be through physical therapy, acupuncture, dry needling, or surgical intervention.
What causes hip impingement?
Understanding the development of hip impingement involves exploring a mix of genetic predispositions and environmental influences. This multifaceted condition, which affects the normal function and movement of the hip joint, can stem from various sources.
Genetic Factors
Hereditary Traits: Some individuals are born with or develop structural irregularities in their hip joints due to genetic factors. These can include variations in the shape of the femoral head, the depth of the acetabulum, or the overall alignment of the hip joint.
Familial Tendencies: Research suggests that hip impingement can run in families, indicating a genetic component to its development. This predisposition might not lead directly to hip impingement but can increase susceptibility when combined with environmental factors.
Developmental Factors
Childhood Growth Patterns: Sometimes, the way bones and joints develop during childhood can set the stage for hip impingement. Conditions like Legg-Calvé-Perthes disease or slipped capital femoral epiphysis during a child’s growth years can lead to structural changes that predispose the hip to impingement later in life.
Bone Maturation and Development: The hip joint, like many other joints in the body, undergoes significant changes as it matures. Any disruption or anomaly in this process can result in joint structures that are more likely to impinge.
Environmental and Lifestyle Influences
High-Impact Sports and Activities: Athletes involved in sports that require repetitive and high-impact hip movements, such as soccer, ballet, and gymnastics, are at a higher risk. These activities place considerable stress on the hip joint, potentially leading to the development of impingement.
One study found that, “adolescents engaged in high-intensity sports were found to be ten times more likely to have a CAM deformity and impingement than age-matched adolescents not participating in high-intensity sports.”
Occupational Hazards: Certain occupations that involve repetitive hip movements or prolonged postures that stress the hip joint can contribute to the onset of hip impingement.
Trauma and Injury: In some cases, a direct injury to the hip can lead to impingement. This might be the result of an accident, a fall, or a sports injury, where the immediate damage eventually leads to long-term structural changes in the hip joint.
Repetitive Motion and Overuse
Muscle Overload: Consistent overuse or strain on the muscles around the hip joint can lead to muscular imbalances. These imbalances might not directly cause hip impingement but can exacerbate the condition if it's already present or developing.
Joint Wear and Tear: Over time, repetitive motion can contribute to the gradual wear and tear of the hip joint, potentially leading to impingement, especially in individuals who are genetically predisposed.
CAM and Pincer Lesions
The complexity of hip impingement, or femoroacetabular impingement (FAI), is often characterized by two distinct types of lesions: CAM and Pincer. These lesions (bony overgrowth), each affecting different parts of the hip anatomy, play a crucial role in the development and progression of hip impingement.
CAM Lesions: The Femoral Neck's Role
Location and Formation: CAM lesions are primarily found on the femoral neck. This area, just below the ball of the hip joint, can develop excess bone growth, leading to a bump-like prominence.
Mechanical Interference: This additional bone growth on the femoral neck can interfere with the smooth articulation between the femur and the acetabulum during movement, particularly during flexion and rotation.
Resulting Damage: The irregular shape caused by CAM lesions leads to abnormal contact with the labrum and cartilage of the acetabulum, causing damage over time. This is especially prevalent during activities that require deep hip flexion or twisting movements.
Prevalence: CAM lesions are more commonly observed in young, active individuals and are particularly associated with athletes. They are believed to result from activities that involve repetitive impact to the growing hip, such as in certain sports during adolescence.
Pincer Lesions: The Acetabulum's Overcoverage
Location and Impact: Pincer lesions occur at the rim of the acetabulum. In these cases, the bone extends beyond the normal boundaries, leading to overcoverage of the femoral head.
Labral Compression: This overcoverage causes the labrum, a ring of cartilage that lines and seals the hip socket, to be compressed. The constant pressing and pinching (hence the term 'pincer') of the labrum can lead to its degeneration and tears.
Joint Damage: Besides labral damage, pincer impingement can also lead to cartilage wear within the acetabulum, contributing to joint degeneration.
Typical Population: Pincer lesions are more commonly seen in middle-aged adults and are more prevalent in women. They can be exacerbated by activities that require a significant range of hip movements.
Combined Impingement: CAM and Pincer Together
Dual Impact: In some cases, individuals can experience both CAM and Pincer lesions simultaneously, known as combined impingement. This combination can cause more complex hip issues due to the dual mechanism of damage – both the excessive bone growth of the femoral neck and the overcoverage of the acetabulum.
Treatment Considerations: Addressing combined impingement typically requires a multifaceted approach, taking into account both types of lesions and their respective impacts on the hip joint.
Hip labral tear diagram
Hip Impingement and Arthritis
The Link Between FAI and Hip Osteoarthritis
Femoroacetabular impingement (FAI) has been increasingly recognized as a significant factor in the development of hip pain and the progression to end-stage hip osteoarthritis. The concept, initially brought to light by Ganz, Leunig, and their colleagues in 2003, highlighted FAI as a critical precursor to degenerative hip conditions. Having FAI does not guarantee that you will have hip osteoarthritis later on in life.
Impact of Abnormal Hip Mechanics
Ganz and team also suggested that a majority of hip osteoarthritis cases, estimated between 70-90%, are likely due to abnormal hip mechanics. These mechanics are often related to conditions such as FAI, hip dysplasia, or other structural deformities in the hip. This insight was pivotal in understanding the etiology of hip osteoarthritis and shifted the focus towards addressing these underlying mechanical issues.
Growth in Treatment and Awareness
Over the last two decades, there has been a significant increase in the awareness and treatment of non-arthritic hip pathologies, including FAI. The field has witnessed an estimated annual growth of 15% in this area, making it one of the fastest-growing segments in sports medicine and orthopedics. This growth reflects a broader recognition of the importance of early intervention and treatment of hip impingement to prevent the progression to osteoarthritis.
Recent Developments
Recent studies and clinical practices continue to support and build upon Ganz and colleagues' initial findings. The focus on early detection and treatment of FAI, particularly in younger and active individuals, aims to preserve the hip joint and delay or prevent the onset of osteoarthritis. This proactive approach in sports medicine and orthopedics underscores the importance of addressing hip mechanics to maintain long-term joint health.
New techniques and less invasive procedures are resulting in better outcomes and faster recovery times for surgical hip impingement cases.
A 2023 study found that a almost 75% of competitive soccer players returned to soccer following hip arthroscopy for femoroacetabular impingement. The study also showed that female and older aged players are less likely to return to play.
Comprehensive Management of Hip Impingement Should Include Acupuncture and Dry Needling
Understanding and managing hip impingement requires a holistic approach that addresses both the symptoms and underlying causes. The integration of acupuncture and dry needling into treatment plans offers a unique and effective strategy to alleviate pain, enhance mobility, and possibly slow down or prevent the progression of hip impingement to more serious conditions such as osteoarthritis or the eventual need for hip replacement. For individuals experiencing hip pain or diagnosed with hip impingement, exploring the benefits of acupuncture and dry needling can be a crucial step in their recovery and journey towards improved hip health.
Over to you
If you liked this article, please share with friends and family who may be suffering with hip impingement or hip pain.
Sources:
Travell, J. G., Simons, D. G. (1993). Myofascial pain and dysfunction: The trigger point manual. London: Lippincott Williams & Wilkins.
Biel, A., & Dorn, R. (2010). Trail guide to the body: A hands-on guide to locating muscles, bones and more. Boulder, CO: Books of Dicovery.
O'Rourke RJ, El Bitar Y. Femoroacetabular Impingement. [Updated 2023 Jun 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK547699/
Fortier, L. M., Popovsky, D., Durci, M. M., Norwood, H., Sherman, W. F., & Kaye, A. D. (2022). An Updated Review of Femoroacetabular Impingement Syndrome. Orthopedic reviews, 14(3), 37513. https://doi.org/10.52965/001c.37513
Shaw C. (2017). Femoroacetabular Impingement Syndrome: A Cause of Hip Pain in Adolescents and Young Adults. Missouri medicine, 114(4), 299–302.
Lee, W. Y., Kang, C., Hwang, D. S., Jeon, J. H., & Zheng, L. (2016). Descriptive Epidemiology of Symptomatic Femoroacetabular Impingement in Young Athlete: Single Center Study. Hip & pelvis, 28(1), 29–34. https://doi.org/10.5371/hp.2016.28.1.29
Tanzer, M., & Noiseux, N. (2004). Osseous abnormalities and early osteoarthritis: the role of hip impingement. Clinical orthopaedics and related research, (429), 170–177.
Packer, J. D., & Safran, M. R. (2015). The etiology of primary femoroacetabular impingement: genetics or acquired deformity?. Journal of hip preservation surgery, 2(3), 249–257. https://doi.org/10.1093/jhps/hnv046
Ganz, R., Parvizi, J., Beck, M., Leunig, M., Nötzli, H., & Siebenrock, K. A. (2003). Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clinical orthopaedics and related research, (417), 112–120. https://doi.org/10.1097/01.blo.0000096804.78689.c2
Rubin, D. (2013). Femoroacetabular Impingement: Fact, Fiction, or Fantasy? American Journal of Roentgenology. Volume 201, Issue 3. https://doi.org/10.2214/AJR.13.10913
Marom, N., Olsen, R., Burger, J. A., Dooley, M. S., Coleman, S. H., Ranawat, A. S., Kelly, B. T., & Nawabi, D. H. (2023). Majority of competitive soccer players return to soccer following hip arthroscopy for femoroacetabular impingement: female and older aged players are less likely to return to soccer. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA, 31(7), 2721–2729. https://doi.org/10.1007/s00167-023-07349-4
Disclaimer: This web site is intended for educational and informational purposes only. Reading this website does not constitute providing medical advice or any professional services. This information should not be used for diagnosing or treating any health issue or disease. Those seeking medical advice should consult with a licensed physician. Seek the advice of a medical doctor or other qualified health professional for any medical condition. If you think you have a medical emergency, call 911 or go to the emergency room. No acupuncturist-patient relationship is created by reading this website or using the information. Morningside Acupuncture PLLC and its employees and contributors do not make any express or implied representations with respect to the information on this site or its use.