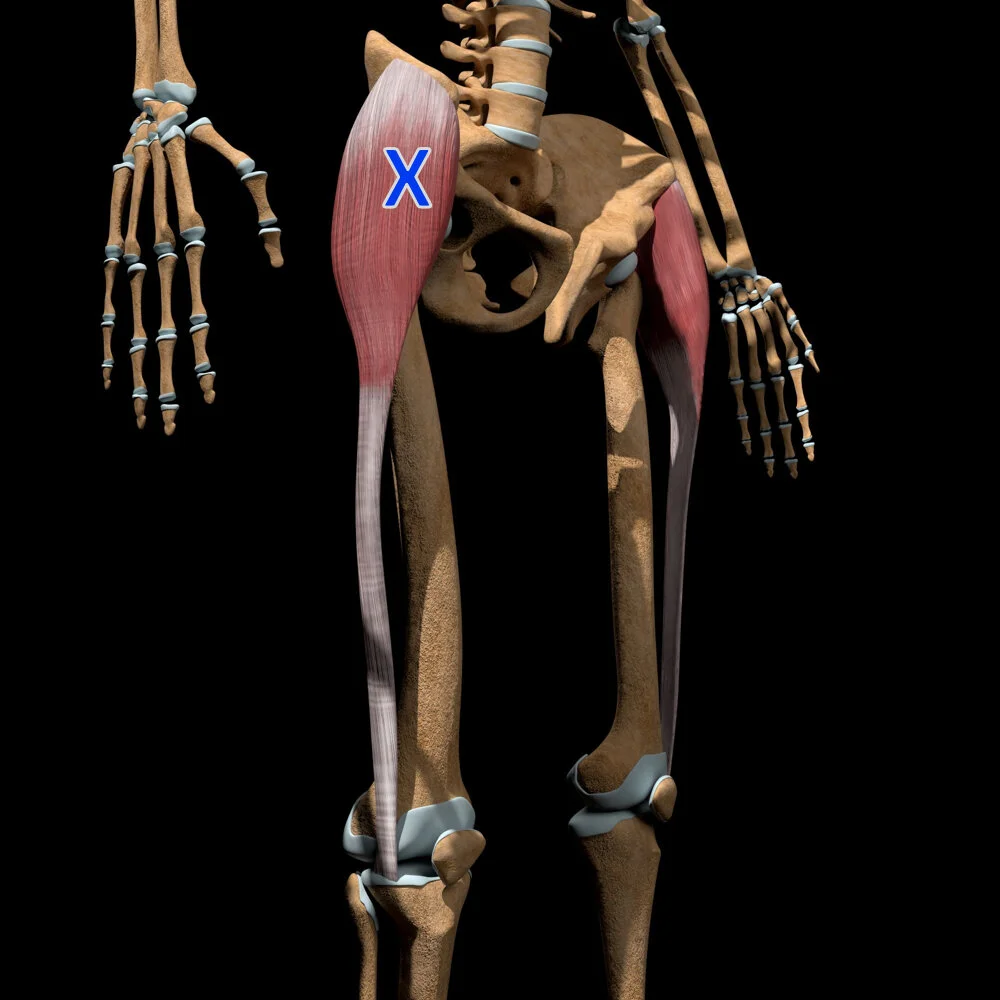
Tensor Fasciae Latae (TFL) Trigger Points
tensor fasciae latae (TFL) muscle trigger points
Introduction
The tensor fasciae latae (TFL) is a hip muscle responsible for hip flexion, abduction, and stabilization. When trigger points develop in this muscle, they can cause hip pain, outer thigh tightness, and knee discomfort, often mimicking iliotibial (IT) band syndrome, hip bursitis, or nerve compression.
Name and Area
Name: Tensor Fasciae Latae (TFL)
Area: Located in the lateral hip, running from the anterior iliac crest to the iliotibial (IT) band.
Indications
TFL trigger points may contribute to:
Pain on the Outer Hip and Thigh (Mistaken for IT Band Syndrome or Hip Bursitis)
Pain That Extends to the Outer Knee (Can Mimic Lateral Knee Pain or Patellar Tracking Issues)
Tightness in the Hip That Restricts Movement (Common in Runners, Cyclists, and Athletes)
Pain or Discomfort When Standing on One Leg or Walking Long Distances
Pain That Worsens with Running, Climbing Stairs, or Lateral Movements
Knee Pain That Feels Worse When Sitting for Long Periods or Descending Stairs
Pain from this muscle is often mistaken for IT band syndrome, hip bursitis, or lateral knee dysfunction.
Muscle Action
Flexes the Hip: Raises the thigh forward, essential for walking, running, and climbing stairs.
Abducts the Hip: Moves the thigh outward, helping with side-to-side stability.
Tenses the IT Band: Supports knee stability and shock absorption.
The TFL is crucial for hip function, knee stability, and lateral leg support.
Signs and Symptoms
Individuals with TFL trigger points often report:
Pain Along the Outer Hip and Thigh That Feels Like a "Tight Band"
Pain or Weakness When Walking or Running (Can Affect Gait Mechanics and Stability)
Pain That Extends to the Outer Knee and Feels Like IT Band Syndrome
Tightness in the Hip That Restricts Leg Movement, Especially Side-to-Side
Pain or Fatigue in the Thigh After Standing for Long Periods
Pain That Feels Worse After Prolonged Sitting, Running, or Lateral Leg Movements
Pain worsens with prolonged standing, running, or excessive hip flexion.
Perpetuating Factors
Common causes of TFL trigger points include:
Running or Sprinting Without Proper Warm-Up (Can Lead to IT Band Overuse and TFL Tightness)
Weak Glute Muscles (Forces the TFL to Compensate for Hip Stability)
Overuse in Lateral Movements (Common in Tennis Players, Soccer Players, and Runners)
Prolonged Sitting or Standing Without Movement (Can Cause Chronic Tightness in the TFL and IT Band)
Excessive Hip Flexor Activation (Cyclists and Those Who Frequently Cross Their Legs May Develop TFL Tightness)
Trigger Point Referral Pattern
Trigger points in the TFL refer pain to:
The outer hip and thigh (Can Mimic IT Band Syndrome or Hip Bursitis)
The lateral knee (Mistaken for Patellar Tracking Issues or Lateral Meniscus Pain)
The upper glute and iliac crest (Can Resemble Lower Back Pain or Glute Dysfunction)
Pain from this muscle is often confused with IT band syndrome, hip joint dysfunction, or lateral knee pain.
Differential Diagnosis
TFL trigger points may be mistaken for:
IT Band Syndrome (Pain on the Outer Thigh and Knee, Worsens with Running and Stair Descending)
Hip Bursitis (Pain on the Lateral Hip, Can Be Tender to Touch and Worsens with Sleeping on the Affected Side)
Lateral Meniscus Injury (Outer Knee Pain That Worsens with Twisting or Running Movements)
Glute Medius Dysfunction (Hip Pain and Instability, Affects Walking and Single-Leg Balance)
Patellar Tracking Disorder (Knee Pain That Feels Worse with Stairs, Squats, or Running)
A thorough hip, knee, and lower limb examination is necessary to rule out these conditions.
Associated Trigger Points
TFL trigger points often co-exist with:
Gluteus Medius and Minimus (Outer Hip and Buttock Pain, Affects Pelvic Stability and Walking Mechanics)
Vastus Lateralis (Outer Thigh and Knee Pain, Can Mimic IT Band Dysfunction)
Rectus Femoris (Anterior Thigh and Hip Pain, Common in Runners and Those With Hip Flexor Tightness)
Quadratus Lumborum (Lower Back and Hip Pain, Contributes to Postural Instability and Pelvic Imbalances)
Anatomy and Innervation
| Muscle | Origin | Insertion | Innervation |
|---|---|---|---|
| Tensor Fasciae Latae (TFL) | Iliac crest, ASIS | Iliotibial band (IT band) | Superior gluteal nerve (L4–S1) |
The TFL is innervated by the superior gluteal nerve (L4–S1), which also controls hip flexion, abduction, and lateral stability.
Patient Examination
A comprehensive examination should include:
Palpation: Identify tender nodules along the outer hip and lateral thigh.
Resisted Hip Flexion and Abduction Testing: Assess pain and weakness when lifting the knee or leg outward against resistance.
Gait and Postural Analysis: Look for hip instability, excessive lateral movement, or altered stride mechanics.
IT Band and Knee Stability Testing: Rule out ligament injuries, patellar dysfunction, or IT band tightness.
Corrective Actions
Dry Needling
Dry needling can release trigger points in the TFL, reducing thigh tightness and improving hip function.
Manual Therapy
Trigger Point Release: Apply deep sustained pressure to tight spots in the outer hip and thigh.
Massage Therapy: Helps improve circulation and reduce TFL muscle tension.
Stretching
Standing IT Band and TFL Stretch: Cross one leg behind the other and lean away from the affected side to stretch the TFL and IT band.
Foam Rolling the Outer Thigh: Helps reduce IT band tightness and improve TFL flexibility.
Strengthening Exercises
Glute Bridges: Strengthens the glutes to counterbalance TFL tightness and improve hip stability.
Side-Lying Hip Abductions: Improves glute medius activation and reduces overuse of the TFL.
Monster Walks With Resistance Bands: Helps improve lateral hip strength and reduce knee strain.
Postural and Movement Adjustments
Avoid Excessive TFL Overuse (Strengthen the Glutes to Prevent TFL Compensation)
Ensure Proper Running and Walking Mechanics (Engage the Core and Glutes to Reduce IT Band Strain)
Use Proper Footwear for Running and Sports (Prevents Lateral Knee and Hip Dysfunction)
Conclusion
The TFL plays a crucial role in hip flexion, knee stability, and lateral leg function, but trigger points in this muscle can cause significant outer hip, thigh, and knee pain. By incorporating dry needling, manual therapy, stretching, and strengthening exercises, individuals can reduce pain, improve mobility, and prevent IT band dysfunction.
➡️ Learn more about Trigger Points
➡️ Explore our Trigger Point Index
Sources:
Travell, J. G., & Simons, D. G. (1983). Myofascial Pain and Dysfunction: The Trigger Point Manual (2nd ed.). Williams & Wilkins.
Simons, D., & Travell, J. (1999). The Trigger Point Manual, Volume 2: The Lower Extremities. Williams & Wilkins.