Back MRI Findings That Don’t Always Mean Pain
Summary of 2025 Dynamic Dry Needling for Neck Pain Study
Your MRI Might Look “Bad” Even If You Have No Back Pain
What a major 2015 review found about disc bulges, degeneration, and other “abnormalities” in symptom-free people
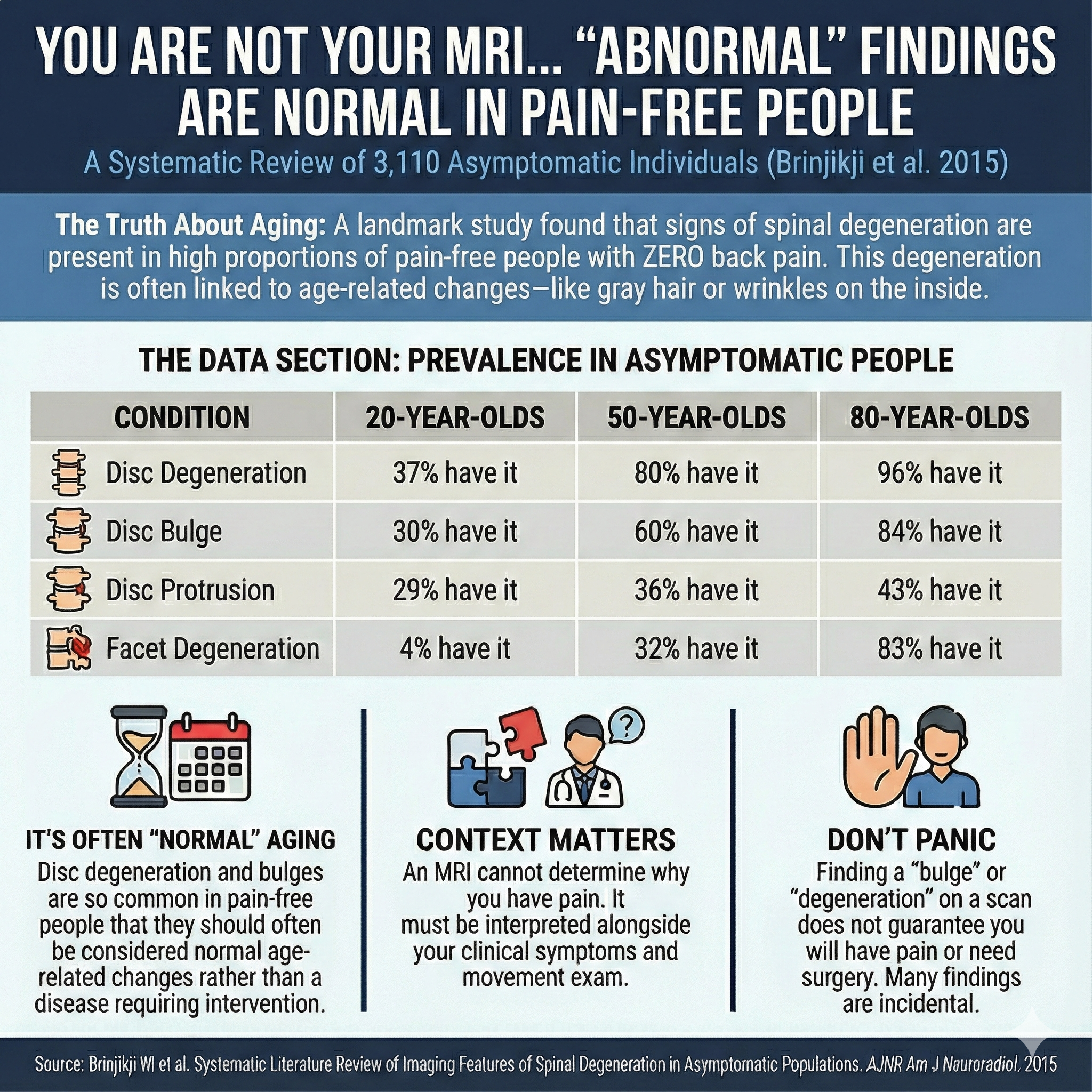
If you’ve ever read an MRI report that mentioned “degenerative disc disease,” “disc bulge,” or “facet arthropathy,” it can feel like you’ve been handed a clear explanation for your pain. The catch is that many of these findings are very common in people who have no low back pain at all.
A large 2015 systematic review and meta-analysis looked at how often common degenerative spine findings show up on MRI or CT in asymptomatic people. The results are a helpful reminder that imaging can be useful, but it’s not the same thing as a diagnosis.
And even when you do have back pain plus an MRI finding, conservative first-line treatments like acupuncture and dry needling can be clinically informative, because a meaningful response suggests your symptoms may be driven more by treatable, modifiable pain mechanisms than by the structural wording on the report (with the caveat that improvement doesn’t “prove” the finding is irrelevant).
Key Points
Many MRI findings labeled “degenerative” are common age-related changes and often appear in people without pain.
Several findings rise steadily with age, including disc degeneration, disc bulge, disc height loss, facet degeneration, and spondylolisthesis.
Imaging is best interpreted alongside your symptoms, exam, function, and response to treatment, not on its own.
Conservative care is often a reasonable first step for many types of low back pain. If symptoms improve, that’s meaningful clinically, but it does not “prove” what did or didn’t cause the pain.
The Study We’re Summarizing: How “Abnormal” Are Normal Spine MRIs?
Paper: Brinjikji et al. (2015), full text on PMC
Before we talk about treatment, we need to get honest about what an MRI can and can’t tell you. This paper is one of the most useful “reality checks” because it answers a simple question:
The Core Question
If you image the spines of people who have no back pain, what do you find? Asymptomatic Low Back MRI Study…
That framing matters because MRI reports often read like a list of problems, and it’s easy to assume every finding is the cause.
Why This Review Was Needed
The authors point out a common problem in back pain care: imaging findings like disc degeneration, facet hypertrophy, and disc protrusions are often interpreted as “the reason” someone hurts, which can trigger treatments that don’t always help. Asymptomatic Low Back MRI Study…
So the practical goal here wasn’t to say imaging is bad. It was to give clinicians and patients a baseline: how common are these findings when pain isn’t present? Asymptomatic Low Back MRI Study…
What “Asymptomatic” Actually Means Here
“Asymptomatic” in this review means people who did not have back pain symptoms (based on the included studies’ definitions). That doesn’t mean their spines were “perfect,” and it doesn’t mean they never had a stiff day in their lives. It means they weren’t presenting as back pain patients in the way we usually think about clinically.
This matters because it reframes a lot of MRI language as common structural variation rather than automatic pathology.
How They Did the Study (So We Can Trust the Numbers)
1) They searched broadly, then narrowed hard
Their search produced 379 unique articles, and after screening and exclusions, 33 studies met criteria, representing 3,110 asymptomatic individuals. Asymptomatic Low Back MRI Study…
2) They didn’t just “average” results
They modeled prevalence by decade using a generalized linear mixed-effects model, producing estimates at ages 20, 30, 40, 50, 60, 70, and 80. Asymptomatic Low Back MRI Study…
3) What did they measure?
They focused on findings that show up constantly in MRI reports:
Disc degeneration
Disc signal loss (“black disc”)
Disc height loss
Disc bulge
Disc protrusion
Annular fissure
Facet degeneration
Spondylolisthesis Asymptomatic Low Back MRI Study…
This is basically the “usual suspects” list in spine imaging.
What They Found (With the Clinical Meaning)
The headline: “Degeneration” is common without pain
Their conclusion is direct: imaging features of degeneration are present in high proportions of people without symptoms and increase with age. Asymptomatic Low Back MRI Study…
That’s the key shift: a finding can be real, measurable, and still not be the reason someone hurts.
But the more useful story is in the pattern
This isn’t just “everything is normal.” Different findings behave differently:
Findings that rise a lot with age (common “normal aging” signals)
Disc degeneration climbs from 37% at age 20 to 96% at age 80. Asymptomatic Low Back MRI Study…
Disc bulge rises from 30% at age 20 to 84% at age 80. Asymptomatic Low Back MRI Study…
Facet degeneration starts low in younger decades and increases sharply later. Asymptomatic Low Back MRI Study…
Spondylolisthesis is uncommon until later decades and becomes much more common after 60. Asymptomatic Low Back MRI Study…
This is why a report can sound scary while describing something that’s statistically common.
Findings that don’t change much with age (and may be less specific)
Disc protrusion and annular fissure are “moderately prevalent” across age categories and don’t rise dramatically with age. Asymptomatic Low Back MRI Study…
That doesn’t mean they never matter. It means their presence alone doesn’t cleanly explain symptoms.
The Most Important Line for Patients Reading Their MRI
The authors explicitly say that when these findings are incidentally seen, they should often be considered normal age-related changes rather than automatic pathology requiring intervention. Asymptomatic Low Back MRI Study…
This is the sentence that should be stapled to a lot of MRI reports.
The Curious Question: Which MRI Findings Do Tend to Correlate With Pain?
This is where patients deserve a more nuanced answer than “imaging doesn’t matter.”
Pain isn’t one thing. Clinically, we usually separate:
Axial low back pain (mostly back-centered pain, stiffness, ache)
Radicular pain (leg-dominant pain, often with numbness/tingling, worse with cough/sneeze, sometimes weakness)
Stenosis-type symptoms (walking intolerance, heaviness, relief with sitting/flexion)
Inflammatory patterns (morning stiffness improving with movement, night pain, systemic clues)
So what tends to correlate better?
In general, imaging correlates better when symptoms are specific
This paper’s discussion notes that prior work has found degenerative findings aren’t necessarily associated with the presence or intensity of low back pain. Asymptomatic Low Back MRI Study…
But it also highlights something more specific: one study they cite found disc herniations were strongly associated with low back pain severity among young adults, while several other findings (annular fissures, high-intensity zones, Modic changes, spondylotic defects) were not associated with severity in that study. Asymptomatic Low Back MRI Study…
That aligns with what many clinicians see: when imaging “matters most,” it’s often because it matches a clear symptom pattern, not because it exists.
A better way to ask the MRI question
Instead of “What did my MRI show?” the more useful questions are:
Does the finding match where my symptoms actually are? Asymptomatic Low Back MRI Study…
Do I have leg symptoms that map to a nerve root pattern?
Do I have objective neurologic signs (weakness, reflex changes, sensory loss)?
Does my pain behave like mechanical sensitivity (load, bending, bracing), or like something else?
What happens when we change the inputs: movement, loading, sleep, stress, muscle tone?
Those questions are the bridge between “picture” and “person.”
Why This Study Changes How You Use the Table Below
When you look at your MRI report, the table isn’t there to dismiss your symptoms. It’s there to calibrate your interpretation.
If a finding shows up in a huge percentage of people without pain, then the presence of that finding alone is a weak explanation. What becomes more valuable is:
matching symptom pattern,
exam findings,
and response to conservative treatment.
That’s where acupuncture and dry needling fit in the next section.
| Imaging finding (asymptomatic) | Age 20 | Age 30 | Age 40 | Age 50 | Age 60 | Age 70 | Age 80 |
|---|---|---|---|---|---|---|---|
| Disc degeneration | 37% | 52% | 68% | 80% | 88% | 93% | 96% |
| Disc signal loss | 17% | 33% | 54% | 73% | 86% | 94% | 97% |
| Disc height loss | 24% | 34% | 45% | 56% | 67% | 76% | 84% |
| Disc bulge | 30% | 40% | 50% | 60% | 69% | 77% | 84% |
| Disc protrusion | 29% | 31% | 33% | 36% | 38% | 40% | 43% |
| Annular fissure | 19% | 20% | 22% | 23% | 25% | 27% | 29% |
| Facet degeneration | 4% | 9% | 18% | 32% | 50% | 69% | 83% |
| Spondylolisthesis | 3% | 5% | 8% | 14% | 23% | 35% | 50% |
If You Have Pain and an MRI Finding, What Do You Do Next?
This study doesn’t say your MRI is irrelevant. It says your MRI finding is not automatically the diagnosis.
So if you have back pain and your report mentions a bulge, degeneration, a protrusion, or facet changes, the next step is not guessing. It’s answering three practical questions that determine whether the finding is likely driving symptoms and what to do about it.
1) Does the MRI finding match your symptom pattern?
MRI findings matter most when they match a specific presentation.
Examples of a stronger match
Pain that travels into the leg in a consistent pattern (often below the knee)
Numbness or tingling in a clear distribution
Weakness or changes in reflexes
Symptoms that behave like nerve irritation (for example, worsened by coughing/sneezing or certain spine positions)
Examples of a weaker match
Pain that stays mostly in the low back, shifts side to side, or changes day to day
Stiffness and tightness that feel worse with stress, poor sleep, long sitting, or sudden spikes in activity
A report full of degenerative language without a clear symptom pattern that fits it
This doesn’t “rule in” or “rule out” anything by itself. It just tells you how confident you should be that the MRI finding is the main driver.
2) Are there signs that change the urgency?
Most low back pain improves with conservative care. But certain patterns deserve a faster medical evaluation.
Examples include:
Progressive weakness
Severe numbness
New bowel/bladder changes
Symptoms that are rapidly worsening or not behaving like typical mechanical back pain
If none of that is present, conservative care is usually a reasonable first step.
3) What happens when you test conservative treatment?
This is where many patients get stuck, because they assume the MRI finding means the solution must be structural.
In reality, conservative care often functions like a “stress test” for your symptoms:
If pain calms down and motion improves, you’ve learned your symptoms are modifiable and you can start rebuilding tolerance.
If symptoms don’t change at all, or worsen in a consistent pattern, that’s useful information too. It may suggest you need a different approach, further evaluation, or a different diagnosis.
That’s why we like starting with treatments that can improve pain and function early without locking you into an invasive pathway.
The simple goal
You don’t need to “erase” the MRI finding to feel better.
You need a plan that:
reduces pain enough to move normally again
improves tolerance to sitting, walking, lifting, and training
helps you identify whether your primary driver is nerve irritation, mechanical sensitivity, muscle guarding, or a mix
That’s where acupuncture and dry needling come in.
Acupuncture for Low Back Pain
Acupuncture is the use of an acupuncture needle (which includes hundreds of styles and techniques). Traditional acupuncture refers to styles like TCM and classical acupuncture that rely on traditional acupoints and meridians.
For many people with low back pain, a conservative approach is reasonable before escalating to invasive options, especially when there are no red flags. The American College of Physicians guideline includes acupuncture among non-drug options that may be considered as part of a first-line strategy, depending on the presentation.
How acupuncture may help (in scientific terms)
Acupuncture may help by:
Modulating pain signaling through peripheral input and spinal cord gating
Influencing brain-level pain processing networks involved in threat, attention, and pain modulation
Reducing protective muscle guarding so movement feels safer again
Supporting down-regulation of stress physiology that can amplify pain sensitivity in some people
This isn’t a claim that acupuncture “fixes” disc structure. It’s a claim that acupuncture may help modify the pain experience and movement tolerance while tissues calm down.
Dry Needling for Low Back Pain
Dry needling focuses on myofascial trigger points and sensitive muscle regions using an acupuncture needle. In low back pain, that often means targeting muscles that commonly contribute to:
Local aching pain
Referred pain into the hip or thigh
Stiffness and movement restriction
Protective spasm that flares with activity
Dry needling may be most useful when it helps you move more normally again and tolerate rehab better, rather than as a stand-alone “fix.”
When Treatment Can Be First-Line and Also Clinically Informative
You asked for a section framing acupuncture and dry needling as not only first-line symptom management, but also “diagnostic.”
Here’s the best evidence-aligned way to say it:
If treatment helps, what does that suggest?
If your pain improves meaningfully with conservative care like acupuncture and or dry needling (often paired with movement and progressive loading), it suggests:
your symptoms are modifiable
your nervous system is capable of “turning down the volume”
your pain may be driven more by irritable, treatable inputs (muscle tone, sensitivity, movement intolerance, stress physiology, local irritation) than by a fixed structural problem that must be “corrected”
This aligns with the core message of the 2015 review: many structural findings exist in people without symptoms, so improvement with conservative care is an important part of the clinical picture.
Caveats (the part that keeps this honest)
A positive response does not prove:
the MRI finding is irrelevant
the disc bulge is unrelated in every way
you’ve identified one single “true cause”
Pain is often multi-factorial. Imaging findings can be incidental, contributory, or unrelated depending on the person and the situation. The safest summary is:
If you improve with conservative care, it’s a strong sign your symptoms are treatable and not solely explained by what the image shows, but imaging still needs to be interpreted with your exam and clinical history.
Practical Takeaway
MRI reports can be useful, but they’re not fortune tellers. This study supports a common-sense approach:
Rule out red flags and major neurologic deficits
Treat what’s treatable first (pain modulation, mobility, muscle sensitivity, graded loading)
Reassess using function, not fear
Use imaging to guide decisions when it’s truly likely to change management
Frequently Asked Questions (FAQ)
If my MRI says “degenerative disc disease,” does that mean my back pain is permanent?
Not necessarily. Degenerative findings are extremely common with age, including in people without pain. PMC
Should I get an MRI right away for low back pain?
Often, no, unless there are red flags or significant neurologic symptoms. Many cases improve with time and conservative care.
Is dry needling the same as acupuncture?
Dry needling is an acupuncture style because it uses an acupuncture needle, but it usually differs in assessment style, point selection logic, and how it’s integrated into treatment planning.
How many sessions does it usually take?
It depends on the case. Many people look for measurable change within the first few visits (pain, ROM, sleep, flare frequency). Longer-standing symptoms usually take longer and benefit from a combined plan.
Ready to Try Acupuncture & Dry Needling?
Whether you’re struggling with acute or chronic pain, acupuncture and dry needling may help restore mobility and reduce pain - quickly and safely.
📍 Conveniently located in New York City
🧠 Experts in trigger point therapy, acupuncture, and dry needling
Book your appointment today with the experts at Morningside Acupuncture, the top-rated acupuncture and dry needling clinic in New York City.
Let us help you move better, feel stronger, and live pain-free.
Additional Resources & Next Steps
Learn More: Visit our Blog for further insights into our treatment approach.
What to Expect: During your initial consultation, we perform a comprehensive evaluation to develop a personalized treatment plan.
Patient Stories: Read testimonials from patients who have experienced lasting relief.
Sources:
Brinjikji, W., Luetmer, P. H., Comstock, B., Bresnahan, B. W., Chen, L. E., Deyo, R. A., Halabi, S., Turner, J. A., Avins, A. L., James, K., Wald, J. T., Kallmes, D. F., & Jarvik, J. G. (2015). Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. AJNR American Journal of Neuroradiology, 36(4), 811–816. Full text
Qaseem, A., Wilt, T. J., McLean, R. M., & Forciea, M. A. (2017). Noninvasive treatments for acute, subacute, and chronic low back pain: A clinical practice guideline from the American College of Physicians. Annals of Internal Medicine, 166(7), 514–530. DOI
Disclaimer: This web site is intended for educational and informational purposes only. Reading this website does not constitute providing medical advice or any professional services. This information should not be used for diagnosing or treating any health issue or disease. Those seeking medical advice should consult with a licensed physician. Seek the advice of a medical doctor or other qualified health professional for any medical condition. If you think you have a medical emergency, call 911 or go to the emergency room. No acupuncturist-patient relationship is created by reading this website or using the information. Morningside Acupuncture PLLC and its employees and contributors do not make any express or implied representations with respect to the information on this site or its use. For any legal interpretation of scope of practice in your state, consult a licensed attorney or regulatory authority.