What is Fascia?
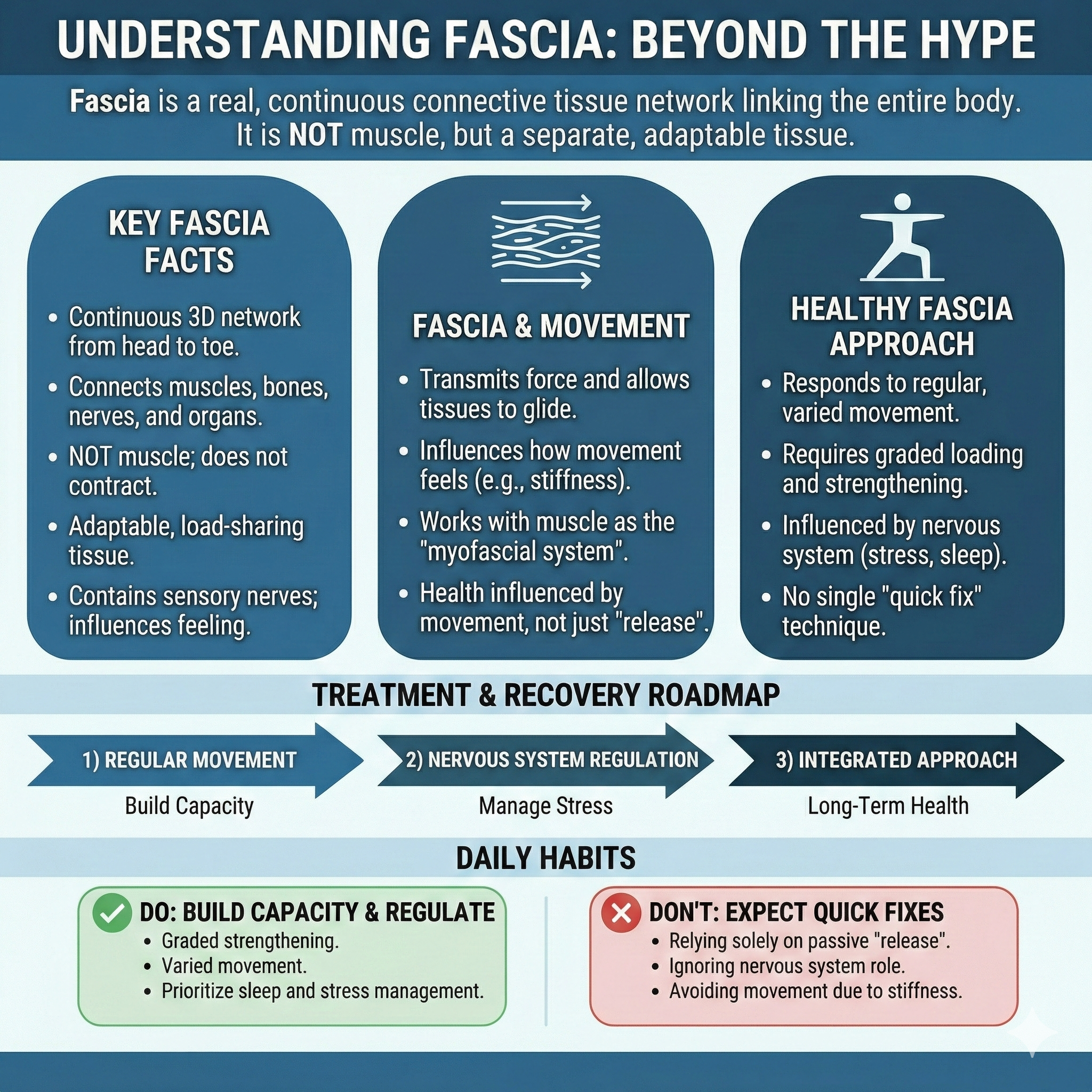
Understanding Fascia Infographic
A Practical, Evidence-Based Explanation of Fascia and the Myofascial System
Fascia has become a popular topic online, often described as the hidden cause of stiffness, pain, or poor mobility. While some claims oversimplify its role, fascia is a real and important tissue with meaningful implications for movement, pain perception, and recovery. Understanding fascia through an evidence-based lens helps separate useful concepts from hype.
Key Points
Fascia is a continuous connective tissue network that links muscles, bones, nerves, and organs throughout the body
It helps transmit force, allows tissues to glide, and contributes to how movement feels
Fascia is not muscle, but it works closely with muscle as part of the myofascial system
Fascia contains sensory nerve endings and may influence stiffness, discomfort, and pain sensitivity
Fascia health is influenced by movement, loading, and nervous system regulation rather than one-off “release” techniques
What Is Fascia?
Fascia is a type of connective tissue that surrounds, separates, and connects structures throughout the body. Rather than existing as isolated sheets, fascia forms a continuous, three-dimensional network extending from head to toe. This network links muscles to one another, connects muscles to bones, and integrates with nerves, blood vessels, and organs.
From a functional perspective, fascia helps organize tissues and allows different layers to move smoothly against each other. It also plays a role in distributing mechanical forces across regions of the body, rather than movement stress being absorbed by a single muscle or joint.
Fascia Is Not “Just Wrapping”
Fascia is sometimes described as passive packing material, but modern research does not support that view. Fascia contains fibroblasts, collagen fibers arranged in specific orientations, and sensory nerve endings. This means fascia is responsive to mechanical input and capable of adapting over time.
Importantly, fascia is not designed to actively contract like muscle. Instead, it behaves as a load-sharing and force-transmitting tissue. When functioning well, fascia contributes to efficient movement and a sense of fluidity. When its behavior changes, people may perceive stiffness or restriction even without obvious muscle injury.
Fascia vs Muscle: Understanding the Difference
Muscle tissue is specialized for contraction and force production. Its primary role is to shorten and lengthen to create movement.
Fascia, by contrast, is connective tissue. Its role is to link muscles together into functional units and help coordinate force across joints and regions. Fascia does not “fire” the way muscle does, but it strongly influences how force is transmitted and how movement feels.
This distinction helps explain why sensations often labeled as “tight muscles” are not always isolated muscular problems. The experience of tightness can reflect a combination of muscle tone, fascial layer glide, connective tissue sensitivity, and nervous system input working together.
Fascia as Part of the Myofascial System
In clinical settings, fascia and muscle are rarely considered in isolation. Instead, they are viewed together as the myofascial system.
The myofascial system reflects how muscles and fascia function as an integrated unit. Muscle contraction places tension into fascial tissues, and fascial tension influences how muscles coordinate and transmit force. This relationship helps explain why symptoms in one area can be influenced by movement or load elsewhere in the body.
For patients, this means stiffness or discomfort may not be caused by a single “tight” structure, but by how the system as a whole is responding to stress, activity, or recovery demands.
Fascia and Sensation
Fascia is innervated, meaning it contains sensory receptors that contribute to proprioception and pain perception. This does not mean fascia is inherently painful, but it does mean changes in fascial sensitivity can influence how movement and pressure are experienced.
When the nervous system is more sensitized due to stress, poor sleep, or cumulative load, the myofascial system may feel stiffer or more uncomfortable without structural damage being present. This is one reason symptoms often fluctuate with lifestyle factors rather than remaining constant.
Why Fascia Matters for Pain and Movement
Understanding fascia helps explain several common clinical patterns:
Stiffness that improves with movement rather than rest
Discomfort that feels diffuse or difficult to pinpoint
Symptoms that shift location during activity
Temporary relief from manual therapy that requires follow-up movement to maintain gains
Rather than viewing fascia as something that becomes “damaged” or “knotted,” a more useful framework is adaptability. Fascia responds to how the body is loaded, how often it moves, and how the nervous system regulates tone and sensitivity.
What This Means for Treatment and Recovery
There is no single intervention that “fixes” fascia. Research and clinical experience both suggest that fascia responds best to a combination of:
Regular, low-intensity movement
Progressive loading through strength and activity
Nervous system down-regulation when stress levels are high
Targeted manual or needling techniques used as adjuncts, not standalone solutions
This systems-based approach aligns more closely with long-term improvement than relying on isolated release techniques alone.
| Topic | Practical takeaway | What to do |
|---|---|---|
| What fascia is | A continuous connective tissue network that links and organizes structures and helps transmit force. | Think “myofascial system,” not isolated tissues. |
| Fascia vs muscle | Muscle creates force; fascia helps distribute and transmit that force across regions. | If stretching isn’t helping, focus on movement + loading instead of more stretching. |
| Why you feel stiff | Stiffness can reflect tone + sensitivity + tissue glide, not just “short muscles.” | Use gentle movement, breathing downshifts, and gradual strengthening. |
| What “release” means | Often a short-term change in comfort, sensitivity, and movement—not permanent tissue remodeling. | Use rolling/massage as a supplement, then reinforce with movement. |
| Best fascia habits | Balanced stiffness and tissue adaptation are supported by consistent training inputs over time. | Walk daily, lift through full ranges, and progress load gradually. |
| When to seek help | If pain is persistent, worsening, or limiting function, you may need an individualized plan. | Get assessed for myofascial contributors, strength deficits, and movement patterns. |
Fascia Research: What the Literature Actually Says
1) Fede et al. (2021) — Fascia biology, innervation, and mechanotransduction
This narrative review explains fascia as a dynamic connective tissue network made of collagen and extracellular matrix, populated by specialized cells (including fibroblasts), and influenced by mechanical loading. A key clinical takeaway is that fascia is innervated and capable of mechanotransduction, meaning mechanical forces can influence cellular signaling and tissue behavior. The paper helps support a practical framework for patients: stiffness and pain aren’t only about “tight muscles,” but may also involve connective tissue sensitivity and how tissues respond to load over time.
2) Kumka & Bonar (2012) — A practical classification system for fascia
This literature review proposes a functional classification of fascial structures to reduce confusion about what “fascia” means, since different tissues are often lumped together under one word. The authors describe fascia as a broad category of connective tissues with distinct roles (for example, tissues that link structures, resist compression, separate layers, or organize fascicles). For patient education, this is useful because it supports a balanced message: fascia is not one single sheet you “release,” but multiple connective tissues with different functions depending on location and role.
3) Colonna et al. (2024) — Fascia, stiffness, and exercise adaptations
This narrative review discusses fascia and the myofascial system in relation to physical exercise, emphasizing the idea of “balanced fascial stiffness” for movement quality and function. A practical takeaway is that tissues adapt differently depending on the type of training. The review highlights that resistance training, aerobic training, plyometrics, and stretching can lead to different changes in tissue stiffness and function over time. For readers, this supports a more evidence-aligned approach than one-off “release” trends: consistent movement and progressive loading may be more meaningful for long-term tissue behavior.
4) Pirri et al. (2025) — Fascia as a potential contributor in complex pain conditions (CRPS)
This narrative review explores fascia’s potential role in Complex Regional Pain Syndrome (CRPS), emphasizing that fascia is highly innervated and may be relevant to pain modulation, sensitization, and inflammatory pathways in complex pain states. This isn’t a “fascia causes CRPS” argument. It’s more of a research-forward perspective that fascia deserves more attention as part of the broader pain science picture. For a general audience, the message is: in some chronic pain conditions, pain can be influenced by nervous system sensitivity and connective tissue signaling, not only by local tissue damage.
5) NCCIH (2023) — Fascia as an under-recognized but important tissue in health and movement
In this director’s message, NCCIH highlights fascia as a long-neglected tissue that is increasingly being studied. The piece emphasizes the interconnected nature of fascia, the concept of the “myofascial unit,” and a practical clinical principle: movement matters, starting gently and progressing as tolerated. It also reinforces that fascia research is still evolving, and that the best public health takeaway right now is consistent, tolerable movement and body awareness rather than extreme “release” claims.
Frequently Asked Questions (FAQ)
Is fascia real, or just a wellness trend?
Fascia is a real connective tissue network studied in anatomy and increasingly in pain and movement research. Social media has amplified interest, but the tissue itself is not new.
Can fascia actually get “tight”?
People commonly use “tight” to describe stiffness or restricted motion. What you feel may reflect a mix of factors: muscle tone, connective tissue glide, sensitivity, and nervous system regulation. The most helpful approach is focusing on movement quality and gradual loading rather than trying to “break adhesions.”
Does stress affect fascia?
Stress can influence the nervous system and increase protective muscle tone and pain sensitivity, which often shows up as stiffness. Fascia is innervated, so it may be part of why the body feels different under stress, even without injury.
Do foam rolling and massage “release fascia”?
They may temporarily change sensation, comfort, and range of motion for some people. Many clinicians view these tools as short-term symptom modifiers that work best when paired with movement and strengthening so the benefits hold.
What’s the best daily habit for fascia health?
Consistent low-intensity movement (like walking) plus progressive strengthening tends to be more reliable long-term than chasing constant “release.”
How does dry needling relate to fascia?
Dry needling uses an acupuncture needle to stimulate myofascial trigger points and sensitive tissue interfaces. Many people experience improved motion and reduced protective tone afterward, especially when it’s followed by movement retraining and progressive loading. (We’ll cover this in detail in the next posts in this series.)
Ready to Try Acupuncture & Dry Needling?
Whether you’re struggling with acute or chronic pain, acupuncture and dry needling may help restore mobility and reduce pain - quickly and safely.
📍 Conveniently located in New York City
🧠 Experts in trigger point therapy, acupuncture, and dry needling
Book your appointment today with the experts at Morningside Acupuncture, the top-rated acupuncture and dry needling clinic in New York City.
Let us help you move better, feel stronger, and live pain-free.
Additional Resources & Next Steps
Learn More: Visit our Blog for further insights into our treatment approach.
What to Expect: During your initial consultation, we perform a comprehensive evaluation to develop a personalized treatment plan.
Patient Stories: Read testimonials from patients who have experienced lasting relief.
Sources:
Fede, C., Pirri, C., Fan, C., Petrelli, L., Guidolin, D., De Caro, R., & Stecco, C. (2021). A closer look at the cellular and molecular components of the deep/muscular fasciae. International Journal of Molecular Sciences, 22(3), 1411. https://pmc.ncbi.nlm.nih.gov/articles/PMC7866861/
Kumka, M., & Bonar, J. (2012). Fascia: A morphological description and classification system based on a literature review. Journal of the Canadian Chiropractic Association, 56(3), 179–191. https://pmc.ncbi.nlm.nih.gov/articles/PMC3430451/
Colonna, S., Casacci, P., & Stecco, C. (2024). Myofascial system and physical exercise: A narrative review. [PMC full text]. https://pmc.ncbi.nlm.nih.gov/articles/PMC11755199/
Pirri, C., Stecco, A., Petrelli, L., & Stecco, C. (2025). An emerging perspective on the role of fascia in complex regional pain syndrome: A narrative review. [PMC full text]. https://pmc.ncbi.nlm.nih.gov/articles/PMC11942918/
National Center for Complementary and Integrative Health. (2023, September 27). Article spotlights an often-neglected part of the body. https://www.nccih.nih.gov/about/offices/od/director/past-messages/article-spotlights-an-often-neglected-part-of-the-body
Disclaimer: This web site is intended for educational and informational purposes only. Reading this website does not constitute providing medical advice or any professional services. This information should not be used for diagnosing or treating any health issue or disease. Those seeking medical advice should consult with a licensed physician. Seek the advice of a medical doctor or other qualified health professional for any medical condition. If you think you have a medical emergency, call 911 or go to the emergency room. No acupuncturist-patient relationship is created by reading this website or using the information. Morningside Acupuncture PLLC and its employees and contributors do not make any express or implied representations with respect to the information on this site or its use. For any legal interpretation of scope of practice in your state, consult a licensed attorney or regulatory authority.