Fascia and the Nervous System
Fascia and the Nervous System
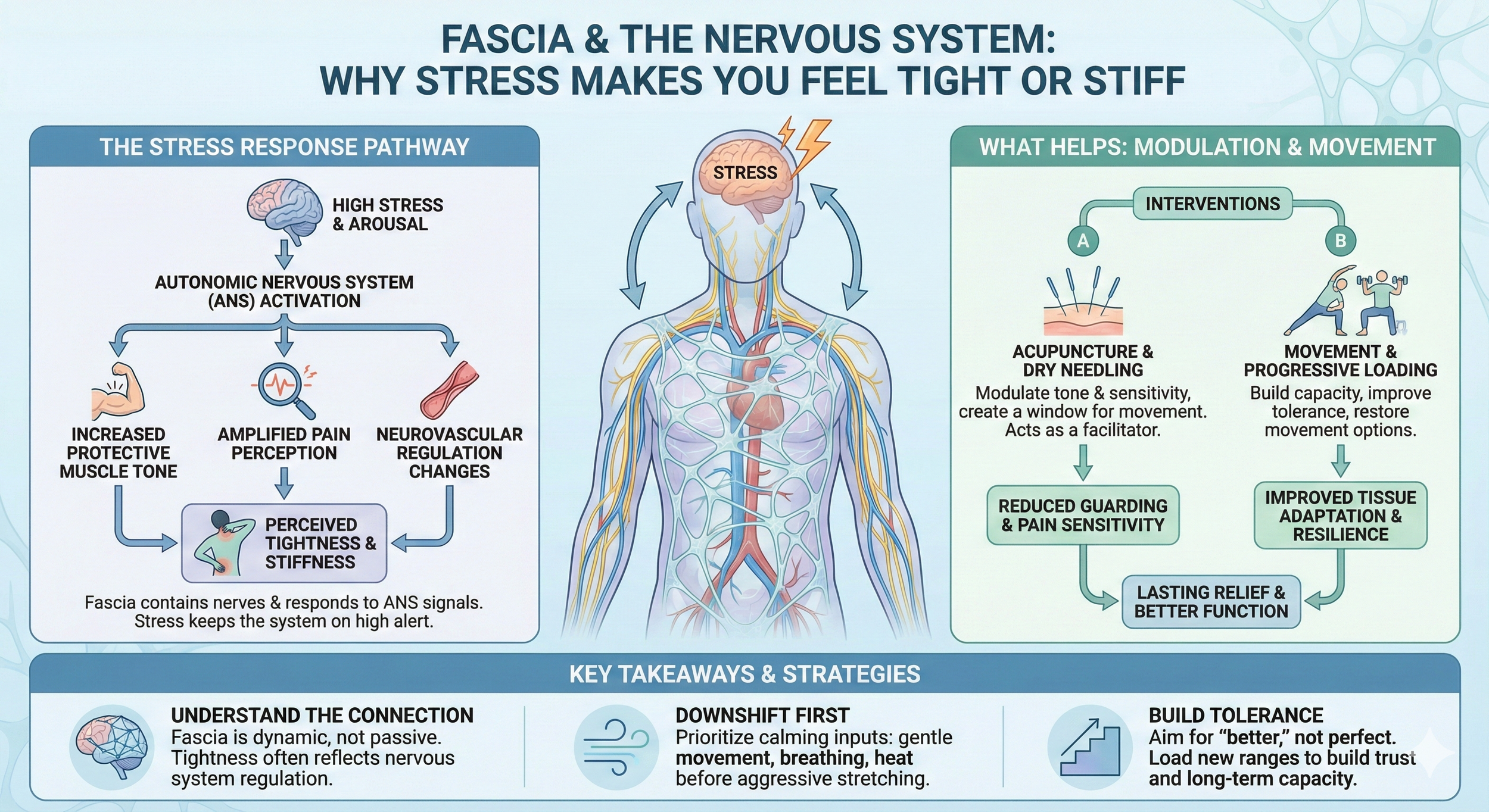
Why Stress Can Make You Feel Tight or Stiff
If your body feels tighter during stressful weeks, you’re not imagining it. Fascia is an innervated, living connective tissue network, and its behavior is tightly linked to nervous system regulation. This post breaks down what “stress-related tightness” actually means in scientific terms and what tends to help when stiffness is driven more by sensitivity and protective tone than by structural damage.
Key Points
Fascia is not inert “wrapping.” It’s a dynamic connective tissue network that contains nervous fibers and responds to stimuli
Stress can increase protective muscle tone and amplify pain perception, which often feels like tightness
Fascia is integrated with the autonomic nervous system, including neurovascular regulation
Stiffness that fluctuates day-to-day often reflects sensitivity and regulation, not tissue shortening
Acupuncture and dry needling may help by modulating pain sensitivity and tone, especially when paired with movement and progressive loading
Related Posts:
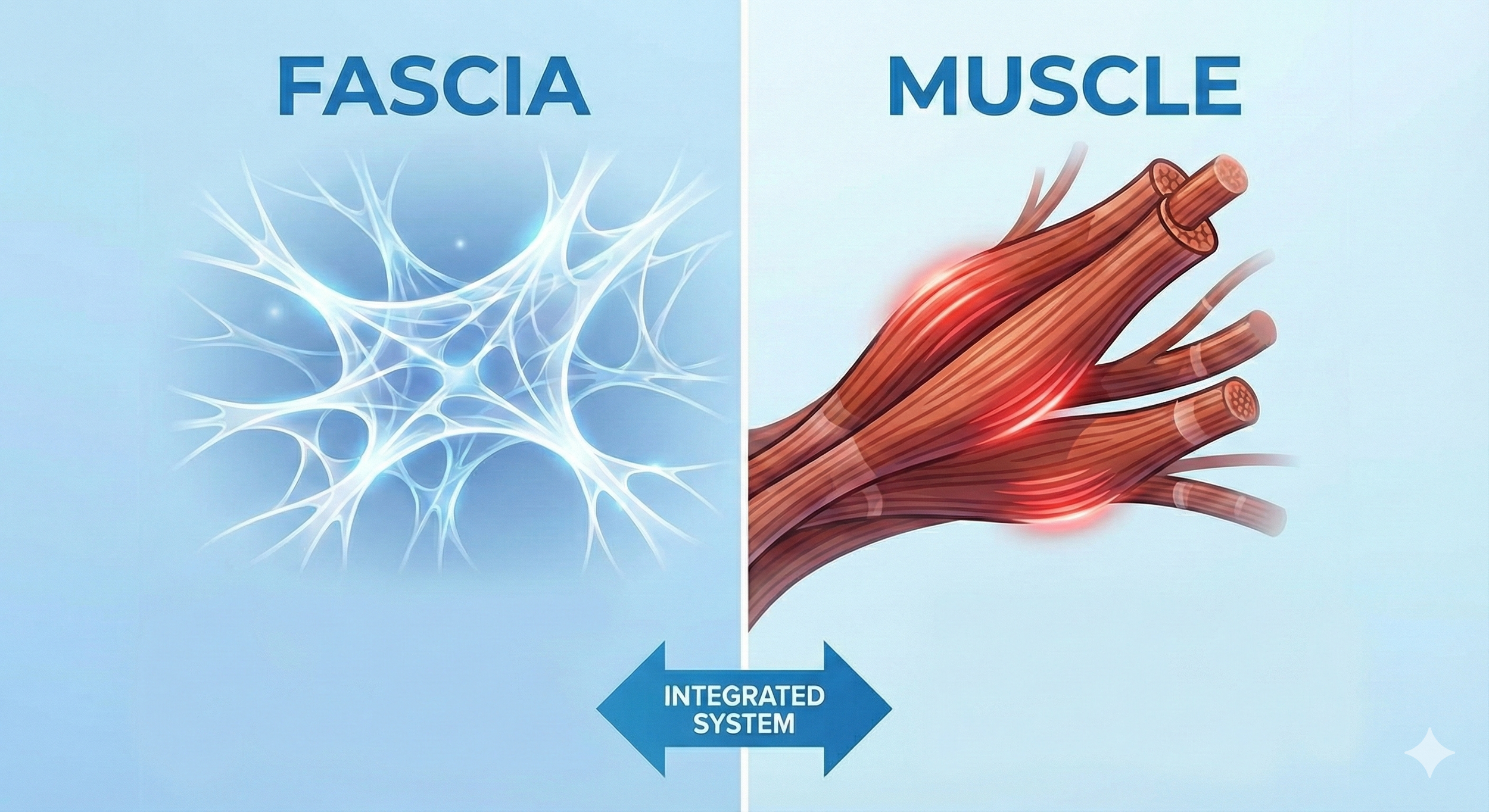
Fascia Is Connected to the Nervous System, Literally
A lot of “fascia content” online treats it like a stuck sheet of plastic wrap. The research picture is more interesting and more clinically useful.
A cellular and anatomical review describes fascia as a dynamic, complex connective tissue network made of cells embedded in the extracellular matrix and nervous fibers, with components that change and respond to stimuli . That matters because it supports a realistic explanation for why the myofascial system can feel different depending on load, recovery, and stress level.
Another key point is that fascia doesn’t just have sensory nerves. It’s also integrated with autonomic regulation. In a narrative review focused on fascia in CRPS, the authors describe autonomic innervation around fascial vasculature and discuss how fascia’s vascularization is “deeply integrated” with the autonomic nervous system and includes sympathetic modulation of vasomotor responses . You don’t need CRPS to find this relevant. The takeaway is that fascia is part of a living neurovascular system, not a passive structure.
Why this matters for patients: If fascia is innervated and neurovascularly regulated, then “tightness” can reflect changes in tone and sensitivity as much as it reflects mechanical stiffness.
Read more: What is Fascia?
A Quick Nervous System Primer for Stress-Related Tightness
Most readers benefit from a simple map:
1) Your nervous system sets your “baseline tension”
Even at rest, muscles have some background tone. That tone is constantly adjusted based on context: fatigue, pain, perceived threat, temperature, and yes, psychological stress. When stress is high, the body often shifts toward a higher-alert state, which can bias the system toward more guarding.
Read more: Fascia vs. Muscle
2) The autonomic nervous system is part of the story
The autonomic nervous system regulates things like heart rate, breathing patterns, and vascular tone. When someone is chronically stressed, their system may spend more time in a heightened state. Because fascia is involved in neurovascular regulation , it makes sense that tissue feel and movement tolerance can shift as autonomic state shifts.
3) Your brain continuously predicts and protects
Pain is not a direct readout of tissue condition. It’s a protective output shaped by sensory input plus the brain’s interpretation of threat and safety. When your system is run down, the threshold for threat can be lower. The result can be stiffness, discomfort, and a reduced tolerance to stretch or pressure without a new injury.
Why Stress Feels Like Tightness Instead of “Stress”
People often say: “I’m stressed, but why does that show up in my hip or neck?”
Here’s the clinically useful framing:
Stress increases arousal and reduces “downshift” time
Arousal tends to increase muscle tone and sensitivity
Fascia is an innervated, stimulus-responsive connective tissue network
So the whole myofascial system can feel tighter, more reactive, and less tolerant to load
This is also why people often notice the same symptom patterns:
“I wake up stiff.”
“It loosens up once I move.”
“It comes back when I sit all day.”
“It gets worse when I’m not sleeping well.”
Those patterns are often more consistent with regulation/sensitivity than with structural shortening.
| What you notice | What it often means | What tends to help |
|---|---|---|
| Tightness spikes during stress | Higher baseline arousal → more protective tone and sensitivity | Downshift inputs (easy movement, breathing), then load gradually |
| Stiff in the morning, better after moving | Myofascial system responds to motion; sensitivity may be higher at rest | Short movement “primer” daily + consistent training inputs |
| Stretching helps briefly, then tightness returns | Stretching doesn’t fully address glide, load tolerance, or guarding | Strength through range + movement variability |
| Diffuse ache or shifting stiffness | Myofascial force transmission + nervous system sensitivity | Myofascial care + progressive loading and recovery |
| Manual therapy helps but doesn’t last | Short-term sensitivity change without reinforcement | Reinforce with targeted exercise in the improved range |
Sensitivity and Pain Perception: The Missing Piece in Most Fascia Content
A huge percentage of fascia conversations skip the most important part: sensitivity.
Peripheral sensitivity: nociceptors and local chemical signaling
In certain conditions, local inflammatory mediators can increase sensitivity of peripheral nociceptors. The CRPS fascia review describes how inflammatory mediators can activate peripheral nociceptors embedded in fascia and how immune mediators can perpetuate nociceptive sensitization . While most readers don’t have CRPS, the mechanism is broadly relevant: tissue sensitivity can change based on local chemical environment and nervous system activation.
Central sensitivity: volume knob turned up
If pain becomes persistent, the central nervous system can become more responsive to signals that would normally be ignored. When that happens, ordinary movement, stretching, or manual pressure can feel excessive. That’s why some people feel “tight everywhere” during stressful periods. It’s not necessarily that the tissue changed overnight. It’s that the system’s sensitivity and tone changed.
Practical takeaway
If tightness improves after calming inputs (easy movement, heat, breathing) and worsens after stress and fatigue, that pattern often points toward sensitivity and regulation rather than purely mechanical stiffness.
Read more about fascia and pain:
https://www.morningsideacupuncturenyc.com/blog/signs-fascia-pain-stiffness
Fascia, Movement, and “Balanced Stiffness”
Stiffness is not always bad. Healthy movement requires a certain amount of stiffness for force transfer and control. The problem is usually maldistributed stiffness (one area over-guarding while another area under-contributes), or stiffness paired with high sensitivity.
Exercise-based fascia literature supports the idea that tissues adapt over time and that different training modalities drive different tissue adaptations. One narrative review cites the concept that even brief targeted work 1–2x/week may stimulate collagen remodeling, and that this renewal process can take months to years . That supports a realistic timeline: durable change usually comes from consistent inputs over time, not one-off release sessions.
Clinical translation:
Short-term: calm sensitivity, reduce guarding, restore movement options
Long-term: build capacity with progressive loading and movement variability
Where Acupuncture and Dry Needling Fit
In musculoskeletal practice, the most useful way to frame acupuncture and dry needling in this context is: they can help modulate tone and sensitivity, creating a window where movement is easier and training is more tolerable.
Dry needling for protective tone and myofascial sensitivity
Dry needling uses an acupuncture needle to stimulate myofascial trigger points and sensitive tissue interfaces. Patients often report a rapid change in movement feel when protective tone is a major driver. When it helps, it’s rarely because tissue was “broken up.” It’s more consistent with a neuromuscular reset and sensitivity modulation.
Acupuncture for pain modulation and nervous system downshifts
Acupuncture is often helpful when symptoms are influenced by stress load, sleep disruption, and global sensitivity. In this context, the needle input is one part of shifting the system toward improved regulation and reduced pain sensitivity, especially when paired with movement and recovery strategies.
The important point
Needling is a facilitator. The gains tend to hold best when you reinforce them with:
easy range-of-motion work
strength through range
progressive loading
recovery habits that reduce baseline arousal
This builds on the fascia vs muscle distinction we wrote about here:
https://www.morningsideacupuncturenyc.com/blog/fascia-vs-muscle
| Approach | Primary clinical role | How it helps fascia & muscle | When it’s most useful |
|---|---|---|---|
| Dry needling | Local myofascial modulation | Targets myofascial trigger points and sensitive tissue interfaces using an acupuncture needle. May reduce protective muscle tone, decrease local sensitivity, and improve short-term movement tolerance. | Localized stiffness, restricted movement, trigger-point–dominant pain, or when tightness limits exercise or rehab progression. |
| Acupuncture | Regional and systemic pain modulation | Influences pain processing and nervous system regulation. May help reduce global sensitivity and normalize tone across the myofascial system. | Widespread stiffness, stress-sensitive symptoms, fluctuating pain, or when recovery and nervous system regulation are limiting progress. |
| Combined approach | Integrated myofascial support | Addresses both local tissue sensitivity and broader nervous system factors. Creates a window where movement and loading feel more accessible. | Persistent or complex symptoms involving both local restriction and global sensitivity, especially in active or high-stress individuals. |
| Needling + movement | Reinforcement of tissue adaptation | Needling reduces protective tone and sensitivity, while movement and strengthening reinforce improved range and load tolerance. | Long-term improvement and prevention of symptom recurrence. |
What Helps When Stress Is Driving Stiffness
This is where readers usually want specifics. Here’s the approach that tends to work clinically:
1) “Downshift first” before chasing flexibility
If your system is upregulated, aggressive stretching can feel like adding threat. Start with:
5–10 minutes of easy walking
gentle mobility in multiple planes
longer exhales or paced breathing
2) Pick one area and improve tolerance, not perfection
Choose the stiffest region and aim for “better,” not “loose.” A small improvement in tolerance often generalizes.
3) Load the range you want to keep
Once motion improves, you need to train it. Otherwise the nervous system often returns to guarding because it doesn’t trust the range under load.
4) Track patterns
If tightness maps onto stress and sleep, treat it like a regulation issue. That’s not dismissive. It’s actionable.
Frequently Asked Questions (FAQ)
Can stress really create physical tightness?
Stress can increase baseline arousal and protective tone. Because fascia is an innervated, stimulus-responsive tissue network , changes in regulation can change how the body feels and moves.
Does this mean my pain is psychological?
No. Stress-related changes are physiological. The nervous system modulates tone, sensitivity, and pain processing, which can make symptoms feel more intense even without new tissue damage.
Why does the tightness move around?
Fascia is part of a continuous connective tissue network, and force transmission can occur across muscle groups and joint regions . Sensitivity also fluctuates, so symptoms can feel variable.
Can fascia actually become inflamed or sensitive?
In certain conditions, inflammatory mediators can contribute to nociceptor activation and sensitization in fascia . For most people, the key takeaway is that sensitivity is modifiable and strongly influenced by movement and recovery.
Where do acupuncture and dry needling fit?
They can be useful tools for reducing protective tone and modulating sensitivity, especially when paired with movement retraining and progressive loading.
Ready to Try Acupuncture & Dry Needling?
Whether you’re struggling with acute or chronic pain, acupuncture and dry needling may help restore mobility and reduce pain - quickly and safely.
📍 Conveniently located in New York City
🧠 Experts in trigger point therapy, acupuncture, and dry needling
Book your appointment today with the experts at Morningside Acupuncture, the top-rated acupuncture and dry needling clinic in New York City.
Let us help you move better, feel stronger, and live pain-free.
Additional Resources & Next Steps
Learn More: Visit our Blog for further insights into our treatment approach.
What to Expect: During your initial consultation, we perform a comprehensive evaluation to develop a personalized treatment plan.
Patient Stories: Read testimonials from patients who have experienced lasting relief.
Sources:
Fede, C., Pirri, C., Fan, C., Petrelli, L., Guidolin, D., De Caro, R., & Stecco, C. (2021). A closer look at the cellular and molecular components of the deep/muscular fasciae. International Journal of Molecular Sciences, 22(3), 1411. https://pmc.ncbi.nlm.nih.gov/articles/PMC7866861/
Kumka, M., & Bonar, J. (2012). Fascia: A morphological description and classification system based on a literature review. Journal of the Canadian Chiropractic Association, 56(3), 179–191. https://pmc.ncbi.nlm.nih.gov/articles/PMC3430451/
Colonna, S., Casacci, P., & Stecco, C. (2024). Myofascial system and physical exercise: A narrative review. https://pmc.ncbi.nlm.nih.gov/articles/PMC11755199/
Pirri, C., Stecco, A., Petrelli, L., & Stecco, C. (2025). An emerging perspective on the role of fascia in complex regional pain syndrome: A narrative review. https://pmc.ncbi.nlm.nih.gov/articles/PMC11942918/
National Center for Complementary and Integrative Health. (2023, September 27). Article spotlights an often-neglected part of the body. https://www.nccih.nih.gov/about/offices/od/director/past-messages/article-spotlights-an-often-neglected-part-of-the-body
Disclaimer: This web site is intended for educational and informational purposes only. Reading this website does not constitute providing medical advice or any professional services. This information should not be used for diagnosing or treating any health issue or disease. Those seeking medical advice should consult with a licensed physician. Seek the advice of a medical doctor or other qualified health professional for any medical condition. If you think you have a medical emergency, call 911 or go to the emergency room. No acupuncturist-patient relationship is created by reading this website or using the information. Morningside Acupuncture PLLC and its employees and contributors do not make any express or implied representations with respect to the information on this site or its use. For any legal interpretation of scope of practice in your state, consult a licensed attorney or regulatory authority.