How to Tell If Fascia Is Causing Your Pain or Stiffness
How to Tell if Fascia is Causing Your Pain or Stiffness
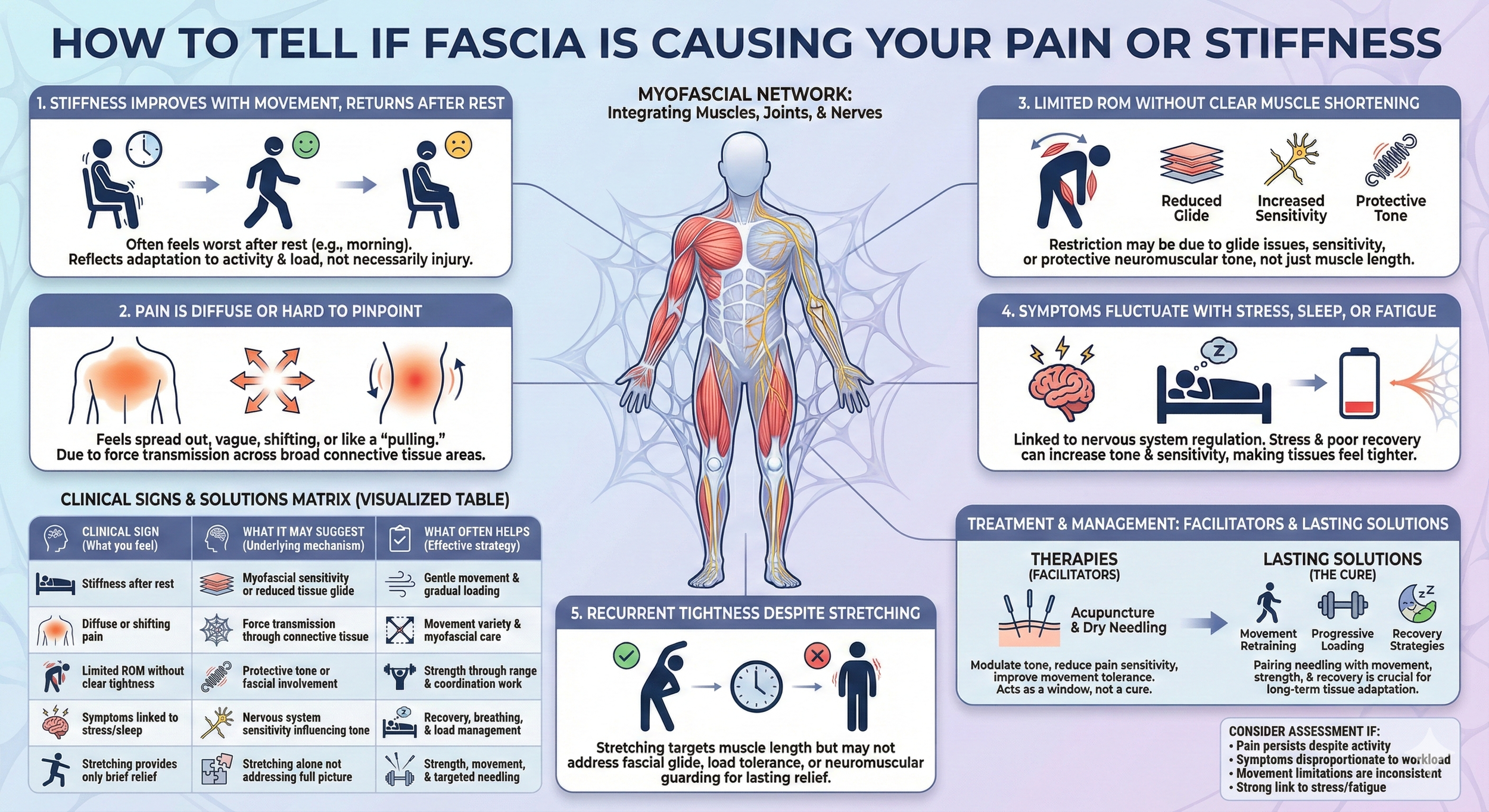
Signs Fascia May Be Contributing to Pain or Stiffness
Many people assume pain or stiffness always comes from “tight muscles,” yet stretching and rest often provide only short-lived relief. In these cases, fascia — the connective tissue network that integrates muscles, joints, and nerves — may be playing a meaningful role. Recognizing when fascia is contributing to symptoms can help guide more effective treatment, movement, and recovery strategies.
Key Points
Fascia-related symptoms often feel diffuse, persistent, or difficult to localize
Stiffness that improves with movement but returns with inactivity may involve myofascial factors
Symptoms are frequently influenced by stress, fatigue, and nervous system sensitivity
Stretching alone may not address fascial glide, load tolerance, or protective tone
Acupuncture and dry needling can help modulate the myofascial system when paired with movement and strengthening
Stiffness That Improves With Movement but Returns Quickly
One of the most common signs fascia may be involved is stiffness that feels worst after rest and improves once movement begins, only to return later in the day or the next morning.
This pattern is frequently seen in the hips, low back, calves, neck, and shoulders. While muscles may be part of the picture, fascia is designed to respond to regular movement and load. When movement variety or tissue loading is limited, people may experience a temporary increase in tissue stiffness or sensitivity rather than structural shortening.
Importantly, this type of stiffness does not necessarily indicate injury. Instead, it often reflects how the myofascial system is adapting to activity levels, recovery, and cumulative load.
Pain or Tightness That Feels Diffuse or Hard to Pinpoint
Fascia connects muscles and structures across regions, which helps explain why fascia-related discomfort often feels spread out, vague, or difficult to isolate to one exact spot.
Patients may describe sensations such as:
A pulling or dragging feeling rather than sharp pain
Discomfort that shifts location with movement
Tenderness that does not match a single muscle belly
This does not mean the pain is “all in your head.” Rather, it reflects how connective tissue transmits force and sensory input across broader areas compared to muscle alone.
This concept builds on the idea of the myofascial system, discussed in detail in our article on what fascia is and why it matters:
https://www.morningsideacupuncturenyc.com/blog/what-is-fascia
Limited Range of Motion Without Clear Muscle Shortening
Some people experience restricted movement even when muscles do not feel overtly short or sore. In these cases, the limitation may be influenced by:
Reduced glide between fascial layers
Increased tissue sensitivity
Protective neuromuscular tone
This helps explain why aggressive stretching sometimes feels uncomfortable or ineffective. Stretching addresses muscle length, but it does not always improve how tissues slide, tolerate load, or respond to neural input.
When range of motion improves temporarily after manual therapy or needling but does not hold, it often suggests the need for follow-up movement and strengthening to reinforce the change.
Symptoms That Fluctuate With Stress, Sleep, or Fatigue
Fascia is innervated and closely linked with the nervous system. As a result, symptoms often fluctuate based on stress levels, sleep quality, and overall recovery rather than activity alone.
When the nervous system is under sustained stress, protective muscle tone and pain sensitivity may increase. This can make tissues feel tighter or more restricted even without structural damage.
This does not mean fascia stores emotions or becomes “knotted” by stress. A more accurate explanation is that nervous system regulation influences how the myofascial system behaves and how strongly sensations are perceived.
Recurrent Tightness Despite Consistent Stretching
If stretching provides only brief relief, fascia may be part of the reason. Stretching primarily targets muscle length but does not reliably address:
Fascial layer glide
Load tolerance
Tissue sensitivity
Neuromuscular guarding
This is why many people feel better immediately after stretching yet return to the same level of stiffness hours later. In these cases, improving movement variety, strength through range, and tissue tolerance tends to produce more durable results.
For a deeper breakdown of this distinction, see our article on fascia vs muscle:
https://www.morningsideacupuncturenyc.com/blog/fascia-vs-muscle
| Clinical sign | What it may suggest | What often helps |
|---|---|---|
| Stiffness after rest | Myofascial sensitivity or reduced tissue glide | Gentle movement and gradual loading |
| Diffuse or shifting pain | Force transmission through connective tissue | Movement variety and myofascial care |
| Limited ROM without clear muscle tightness | Protective tone or fascial involvement | Strength through range and coordination work |
| Symptoms linked to stress or poor sleep | Nervous system sensitivity influencing tissue tone | Recovery, breathing, and load management |
| Stretching provides only brief relief | Stretching alone not addressing full myofascial picture | Strength, movement, and targeted needling |
How Acupuncture and Dry Needling Can Help With Myofascial Symptoms
Acupuncture and dry needling both use solid, filiform needles and are commonly applied in musculoskeletal care to influence the myofascial system rather than isolated tissues.
From a clinical perspective, needling may help by:
Reducing excessive or protective muscle tone
Modulating local pain sensitivity
Improving tolerance to movement
Creating a window where loading and exercise feel more accessible
Dry needling often focuses on myofascial trigger points and sensitive tissue interfaces, while acupuncture may be applied more regionally or systemically depending on presentation. In both cases, needling is best viewed as a facilitator, not a cure.
Lasting improvement typically depends on pairing needling with movement retraining, progressive loading, and recovery strategies that support tissue adaptation.
When to Consider a Myofascial-Focused Assessment
A myofascial-focused evaluation may be helpful when:
Pain or stiffness persists despite regular activity
Symptoms feel disproportionate to workload
Movement limitations are inconsistent or shifting
Stress and fatigue strongly influence symptoms
The goal is not to label fascia as the problem, but to identify how muscle, connective tissue, and the nervous system are interacting and contributing to symptoms.
What the Research Suggests About Fascia, Pain, and Stiffness
Current fascia research helps explain why pain and stiffness do not always behave like simple muscle problems. Across anatomy, exercise science, and pain literature, fascia is increasingly understood as a sensory, load-responsive connective tissue that interacts closely with the nervous system.
Cellular and anatomical research, including the review by Fede et al. (2021), shows that fascia is richly innervated and capable of mechanotransduction. This means connective tissue does not merely transmit force passively. It can respond to mechanical stress and influence sensory input. Clinically, this helps explain why stiffness or discomfort may feel diffuse, persistent, or sensitive to movement and load rather than isolated to one muscle.
Morphological work by Kumka and Bonar (2012) further clarifies that “fascia” is not a single uniform tissue. Instead, it encompasses multiple connective tissues with different structural roles depending on location. This supports why symptoms may present differently in areas like the hips, spine, calves, or shoulders and why simplistic explanations such as “tight fascia” often fall short.
Exercise-focused reviews, including Colonna et al. (2024), emphasize the concept of balanced tissue stiffness. Both muscle and fascia adapt to how they are loaded over time. From this perspective, stiffness itself is not inherently pathological. Problems arise when tissues lose variability, tolerance, or coordinated load sharing, often due to inactivity, repetitive patterns, or insufficient recovery.
Pain-oriented fascia research, such as Pirri et al. (2025), highlights the potential role of connective tissue innervation and nervous system sensitivity in complex pain states. While fascia is not positioned as a sole cause of chronic pain, this work supports a broader model in which tissue sensitivity, neural regulation, and movement interact to shape symptoms.
Finally, perspectives from the National Center for Complementary and Integrative Health (NCCIH, 2023) emphasize that fascia research is still evolving. The most consistent takeaway across disciplines is not aggressive or repeated “release,” but regular movement, gradual loading, and interventions that improve tolerance to motion.
Taken together, the research supports a practical conclusion: when pain or stiffness feels persistent, diffuse, or inconsistent, fascia may be contributing through its interaction with muscle, movement, and the nervous system rather than through structural damage alone.
Frequently Asked Questions (FAQ)
Can fascia be the main cause of pain?
Fascia can contribute to pain perception, particularly through sensitivity and neural input, but it is usually one part of a broader myofascial and nervous system picture.
How is fascia-related stiffness different from muscle soreness?
Muscle soreness is typically localized and activity-specific. Fascia-related stiffness often feels more diffuse, persistent, and influenced by inactivity or stress.
Is foam rolling enough to address fascia issues?
Foam rolling may temporarily reduce discomfort, but longer-term improvement usually requires movement, strengthening, and addressing contributing factors.
Does poor posture damage fascia?
Posture alone is unlikely to damage fascia. However, limited movement variety over time may contribute to stiffness or discomfort.
How long does it take to improve fascia-related symptoms?
Short-term changes may occur quickly, but sustained improvement depends on consistent movement, progressive loading, and recovery habits.
Ready to Try Acupuncture & Dry Needling?
Whether you’re struggling with acute or chronic pain, acupuncture and dry needling may help restore mobility and reduce pain - quickly and safely.
📍 Conveniently located in New York City
🧠 Experts in trigger point therapy, acupuncture, and dry needling
Book your appointment today with the experts at Morningside Acupuncture, the top-rated acupuncture and dry needling clinic in New York City.
Let us help you move better, feel stronger, and live pain-free.
Additional Resources & Next Steps
Learn More: Visit our Blog for further insights into our treatment approach.
What to Expect: During your initial consultation, we perform a comprehensive evaluation to develop a personalized treatment plan.
Patient Stories: Read testimonials from patients who have experienced lasting relief.
Sources:
Fede, C., Pirri, C., Fan, C., Petrelli, L., Guidolin, D., De Caro, R., & Stecco, C. (2021). A closer look at the cellular and molecular components of the deep/muscular fasciae. International Journal of Molecular Sciences, 22(3), 1411. https://pmc.ncbi.nlm.nih.gov/articles/PMC7866861/
Kumka, M., & Bonar, J. (2012). Fascia: A morphological description and classification system based on a literature review. Journal of the Canadian Chiropractic Association, 56(3), 179–191. https://pmc.ncbi.nlm.nih.gov/articles/PMC3430451/
Colonna, S., Casacci, P., & Stecco, C. (2024). Myofascial system and physical exercise: A narrative review. https://pmc.ncbi.nlm.nih.gov/articles/PMC11755199/
Pirri, C., Stecco, A., Petrelli, L., & Stecco, C. (2025). An emerging perspective on the role of fascia in complex regional pain syndrome: A narrative review. https://pmc.ncbi.nlm.nih.gov/articles/PMC11942918/
National Center for Complementary and Integrative Health. (2023, September 27). Article spotlights an often-neglected part of the body. https://www.nccih.nih.gov/about/offices/od/director/past-messages/article-spotlights-an-often-neglected-part-of-the-body
Disclaimer: This web site is intended for educational and informational purposes only. Reading this website does not constitute providing medical advice or any professional services. This information should not be used for diagnosing or treating any health issue or disease. Those seeking medical advice should consult with a licensed physician. Seek the advice of a medical doctor or other qualified health professional for any medical condition. If you think you have a medical emergency, call 911 or go to the emergency room. No acupuncturist-patient relationship is created by reading this website or using the information. Morningside Acupuncture PLLC and its employees and contributors do not make any express or implied representations with respect to the information on this site or its use. For any legal interpretation of scope of practice in your state, consult a licensed attorney or regulatory authority.