Acupuncture for Musculoskeletal Pain Evidence Map
2025 Evidence Review from Frontiers in Medicine
Musculoskeletal pain is a leading cause of disability and lost productivity worldwide. As patients look for non-drug options to manage pain, acupuncture is one of the most studied interventions. A new 2025 evidence map in Frontiers in Medicine synthesized 111 systematic reviews with meta-analyses on acupuncture for 35 musculoskeletal pain conditions, summarizing where the evidence is strong and where gaps remain.
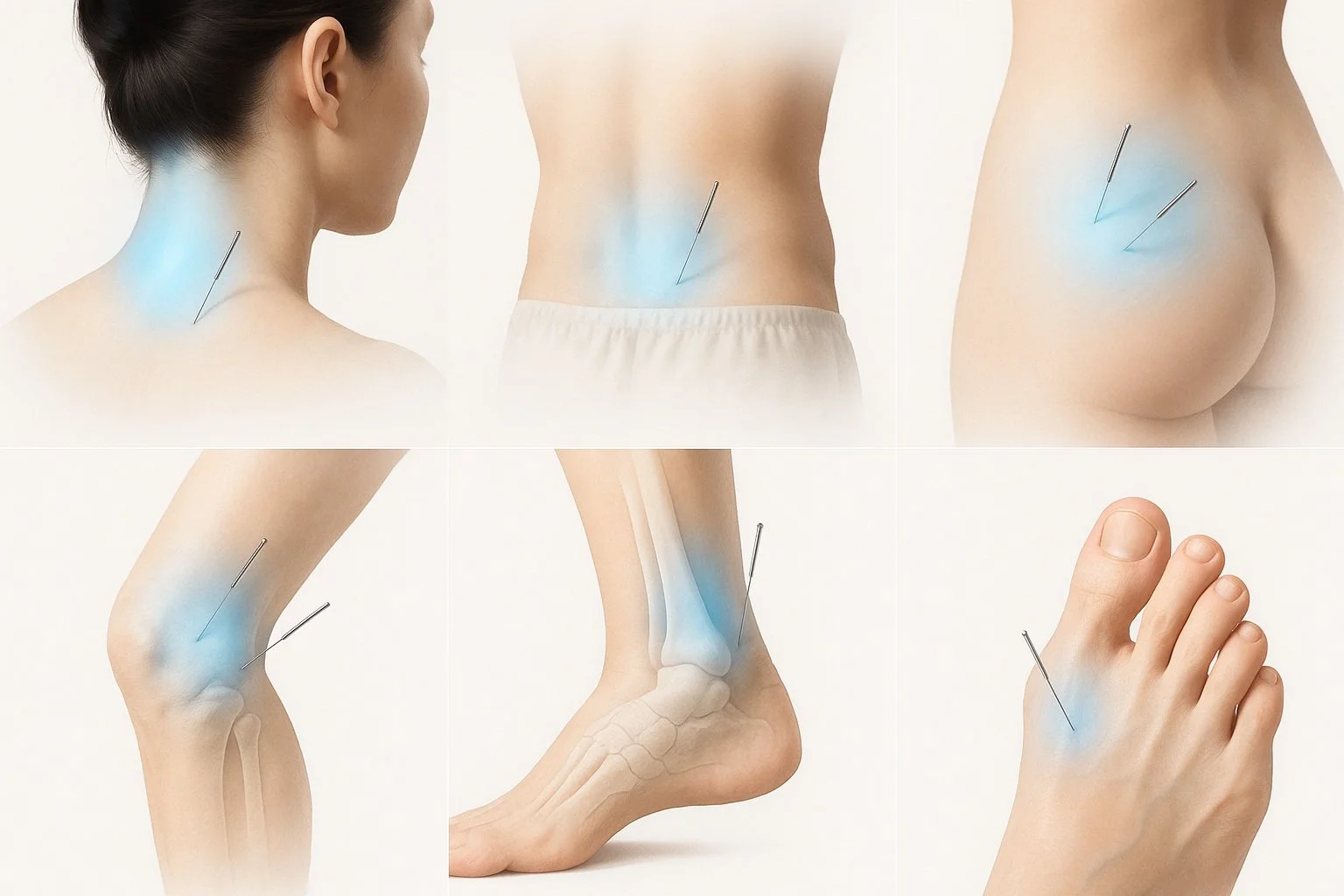
For background on how we approach treatment, see our Acupuncture Guide and our explainer on Acupuncture and the Nervous System.
Studies show acupuncture can help with low back pain, osteoarthritis, neck pain, rheumatoid arthritis, and gout
Key Points
The evidence map included 111 systematic reviews with meta-analysis spanning 35 musculoskeletal pain conditions.
Short-term pain relief favored acupuncture across most major conditions (low back pain, osteoarthritis, neck pain, rheumatoid arthritis, gout).
Long-term effects were positive for some outcomes (notably low back pain), but long-term data are limited overall.
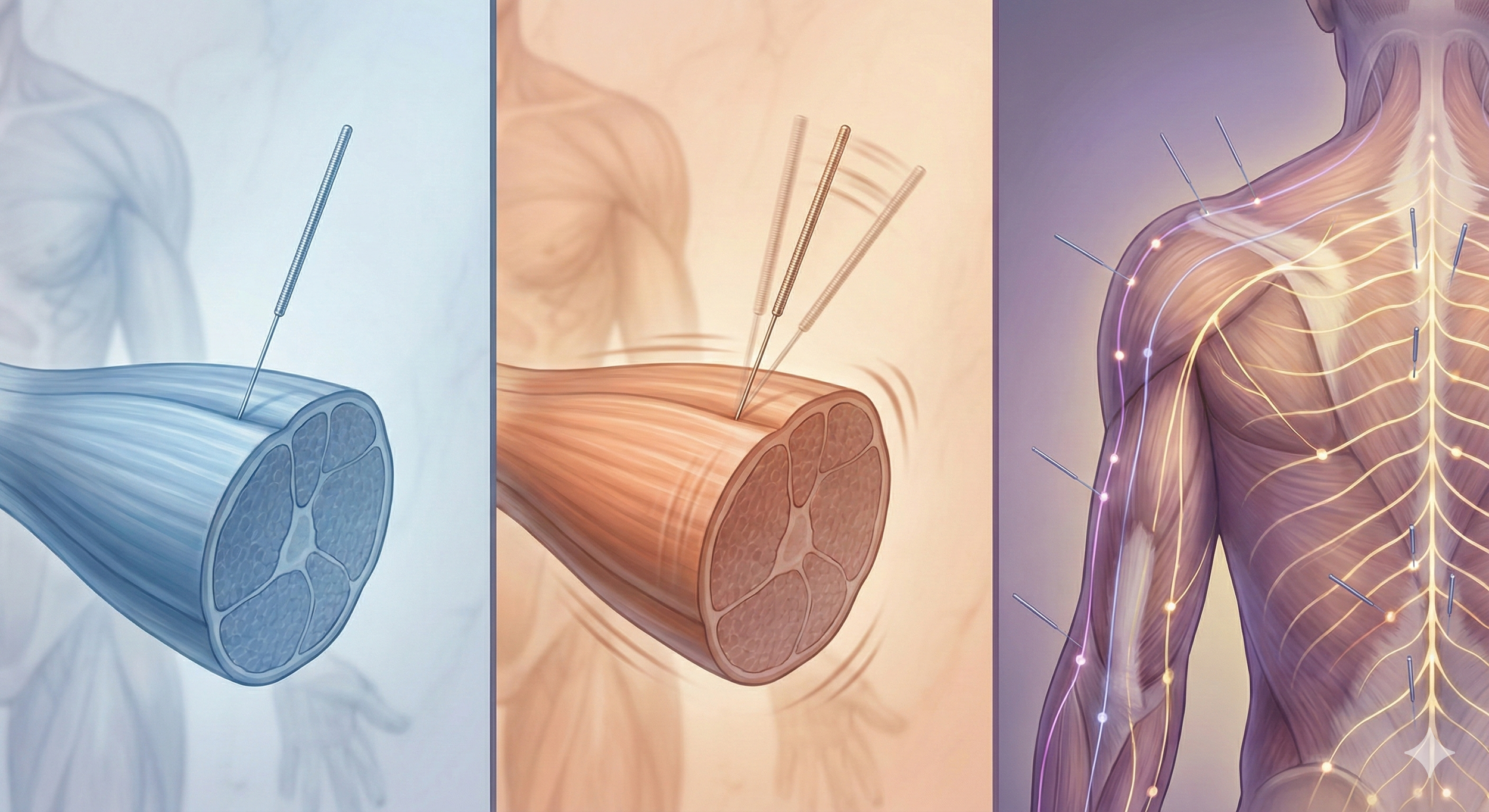
Interventions covered manual acupuncture, electroacupuncture, and warm acupuncture.
Methodological quality of included reviews was mostly low or critically low, so more rigorous trials are needed.
Summary of Acupuncture for Musculoskeletal Pain Research by Condition
| Condition | Short-Term Effects | Long-Term Effects | Acupuncture Types Studied | Key Comparisons | Outcome Summary |
|---|---|---|---|---|---|
| Low Back Pain | Beneficial vs sham, drugs, no treatment, usual care; similar to TENS | Beneficial vs sham and other controls | Manual, Electro, Warm | Sham, drugs, TENS, no treatment, usual care | Strong short-term benefit; sustained benefit reported in follow-ups |
| Osteoarthritis (overall) | Positive vs no-acupuncture controls; mixed vs sham (especially hip OA); some drug comparisons non-significant | Positive vs no-treatment; less clear vs sham | Manual, Electro, Warm | Sham, drugs, usual care, waitlist | Good short-term effects; long-term benefit clearer vs no-treatment than vs sham |
| Knee Osteoarthritis | Beneficial vs sham, drugs, no treatment, usual care, waitlist | Limited but favorable trend | Manual, Electro | Sham, drugs, no treatment | Consistent short-term benefit; needs longer follow-up |
| Hip Osteoarthritis | Beneficial vs drug and control; not significant vs sham | Limited evidence | Manual, Electro | Sham, drugs, control | Mixed findings; more trials needed |
| Neck Pain | Beneficial vs sham/control; some EA studies similar to sham | Similar to sham TENS | Manual, Electro | Sham, drugs, TENS | Short-term benefit common; sparse long-term data |
| Rheumatoid Arthritis | Electroacupuncture beneficial vs sham | Not reported | Electro | Sham | Promising short-term pain relief; limited data volume |
| Gout | Beneficial vs drugs/control | Not reported | Manual, Warm, Electro | Drugs, control | Encouraging early findings; more research needed |
Study Review
(What the authors did, explained)
Design
This was an evidence map, which is a bird’s-eye summary of what research exists on a topic, where the findings point, and where the gaps are. Instead of looking at single trials, the authors only included systematic reviews with meta-analysis about invasive acupuncture for musculoskeletal pain. Invasive means using an acupuncture needle, such as manual acupuncture, electroacupuncture, or warm needle techniques. The goal was to chart patterns across conditions and comparators and visualize them with bubble plots.
Databases and dates
They searched six large medical databases: PubMed, Embase, Cochrane Library, AMED, Web of Science, and Epistemonikos. Searches were run through April 18, 2024, then updated through August 23, 2024 to catch any new publications before analysis. Using multiple databases reduces the chance of missing relevant reviews and the update ensures the map reflects very recent evidence.
Inclusion criteria (what counted) and comparators
To be included, a review had to:
Focus on musculoskeletal pain in any body region.
Evaluate invasive acupuncture: manual acupuncture, electroacupuncture, or warm acupuncture.
Compare acupuncture to controls such as sham acupuncture, no treatment, usual care, or medications/other therapies.
Report pain outcomes on validated scales like VAS or NRS.
They excluded non-needle methods such as acupressure, laser acupuncture, and auricular therapy, and also excluded dry needling as a separate category.
Note: in our materials we may define dry needling as an acupuncture style because it uses an acupuncture needle; the authors chose to categorize it separately for their review criteria.
Scope (how much and what kinds of pain)
The final map included 111 systematic reviews covering 35 distinct musculoskeletal conditions. The most represented were:
Low back pain: 22 reviews
Osteoarthritis: 19 reviews
Neck pain: 6 reviews
Rheumatoid arthritis: 5 reviews
Gout: 4 reviews
The paper also charts many “other” conditions, but these five categories accounted for about half of all included reviews.
Quality (how reliable are the included reviews)
Each review was graded using AMSTAR-2, a standard tool for judging review quality. Results were mostly low or critically low: 23 reviews low and 88 critically low. Common problems included missing lists of excluded studies, not reporting funding sources in the primary trials, and gaps in search strategy reporting. This does not mean acupuncture is ineffective; it means we should be cautious about how strongly we interpret pooled results and that better-designed trials and reviews are needed going forward.
Results
(What they found)
Short-term: Positive effects favored acupuncture for most major conditions and comparators; exceptions included parity with TENS for low back pain and some non-significant findings vs sham in specific OA subgroups.
Long-term: Benefits persisted for low back pain in follow-ups; in osteoarthritis, long-term benefit was clearer vs no-treatment than vs sham; neck pain long-term effects were similar to sham TENS.
Adverse events: Where reported, no major adverse events were identified.
How Acupuncture May Help Musculoskeletal Pain
Listed by condition, with mechanisms
Low Back Pain
Evidence: Beneficial short-term vs sham, drugs, no treatment, and usual care; long-term benefit reported; similar to TENS in some comparisons.
Mechanisms (scientific): Stimulates Aδ/C-fiber afferents → segmental inhibition and central pain modulation; endogenous opioid release; reduced paraspinal muscle guarding; improved local perfusion and movement efficiency.
Summary: Needle-based acupuncture can calm overactive pain nerves, loosen tight back muscles, and improve blood flow. Trials show it usually helps in the short term and sometimes holds up over time. In some studies it worked about as well as TENS.
Osteoarthritis (overall); Knee OA; Hip OA
Evidence: Overall OA: positive vs no-acupuncture controls; mixed vs sham (especially hip OA). Knee OA shows consistent short-term gains; hip OA not significant vs sham in some analyses. Long-term benefit more evident vs no-treatment than vs sham.
Mechanisms: Downregulation of inflammatory mediators such as TNF-α and IL-6; improved periarticular muscle activation and proprioception in knee OA; reduced mechanical stress through better neuromuscular control; enhanced local circulation.
Summary: Acupuncture may lower joint pain by dialing down inflammatory signals and helping the muscles around the joint work more efficiently so the joint is loaded better. Results are strongest for knee OA in the short term. Hip OA findings are mixed when compared to sham. Longer-term benefit is clearer compared with doing nothing than when compared with sham.
Neck Pain
Evidence: Short-term benefit common; electroacupuncture sometimes similar to sham; long-term outcomes similar to sham TENS.
Mechanisms: Modulates dorsal horn transmission; reduces cervical myofascial hyperactivity in muscles like upper trapezius and levator scapulae; improves posture-related muscle imbalance and range of motion.
Summary: Acupuncture often eases neck pain and stiffness by relaxing tight muscles and quieting pain signaling. Longer-term results are less certain, so pairing with exercise or periodic booster sessions may matter.
Rheumatoid Arthritis (pain focus)
Evidence: Electroacupuncture superior to sham for short-term pain relief in limited studies.
Mechanisms: Central analgesia plus autonomic and inflammatory pathway effects, including HPA axis and vagal anti-inflammatory reflex, contributing to symptom relief.
Summary: Electroacupuncture may help reduce RA pain in the short term by calming pain pathways and nudging inflammatory systems toward balance. The evidence base is smaller, so treat these results as promising but preliminary.
Gout
Evidence: Benefits vs drugs and controls, based on a limited number of systematic reviews.
Mechanisms: Pain gating and sympathetic modulation; potential reduction in neurogenic inflammation during flares.
Summary: Gentle acupuncture can help during gout flares by blocking pain signals and calming the stress response. Early studies are encouraging, but there are fewer reviews. Avoid direct needling into the most inflamed spot.
| Condition | Primary Points (Traditional) | Local / Adjunct Points | EA / Technique Notes | Mechanistic Rationale |
|---|---|---|---|---|
| Low Back Pain | BL23, BL25, BL40, GV3, GV4, KI3 | BL26, BL32, BL54, GB30, GB34, Huatuojiaji L3–L5 | EA: BL23↔BL25 or BL40↔GB34 (2–10 Hz) | Segmental inhibition, endogenous opioid release, reduced paraspinal tone, improved perfusion |
| Knee Osteoarthritis | ST35 (Neixiyan), EX-LE4 (Xiyan), GB34, SP9, ST36 | SP10, LR8, KI10, GB33, peri-joint tender points | EA: ST35↔EX-LE4 or GB34↔ST36 (2–10 Hz) | Reduced nociception and inflammation, improved quadriceps activation and proprioception |
| Hip Osteoarthritis | GB29, GB30, GB34, LR3, ST36 | GB31, BL54, KI3; consider gluteus medius/minimus, TFL, piriformis tender points | EA: GB30↔GB34 or local motor points (2–10 Hz) | Decreased periarticular guarding, improved hip mechanics and local circulation |
| Neck Pain | GB20, GB21, LI4, SI3, BL10 | Huatuojiaji C4–C7, SI14, SI15; upper trapezius & levator scapulae tender points | EA: GB20↔GB21 or Huatuojiaji pairs (2–10 Hz) | Dampens myofascial hyperactivity, modulates dorsal horn transmission, reduces referred pain |
| Rheumatoid Arthritis (pain focus) | LI4, LI11, SP6, ST36, LR3 | Local periarticular points by joint (e.g., wrist: TB5, LI5; knee: ST35, GB34) | EA optional at local joints at low frequency, progress by tolerance | Central analgesia with possible autonomic & cytokine modulation supporting symptom relief |
| Gout (acute MTP pain) | LR3, SP6, ST44, KI3 | Local around 1st MTP (avoid direct needling into inflamed capsule) | Gentle manual technique; typically avoid EA in hot, irritable flares | Pain gating, sympathetic modulation, potential reduction in neurogenic inflammatory signaling |
Limitations of the study
Long-term data are scarce because many trials end after 4–12 weeks without extended follow-up.
Review quality issues: Most SRs were rated critically low on AMSTAR-2, often lacking funding source reporting and excluded-study lists.
Geographic concentration: A large share of studies came from Asia, which can limit generalizability.
What this means if you’re considering acupuncture
Acupuncture is a low-risk, non-drug treatment that may reduce pain and improve function for common conditions like low back pain, knee osteoarthritis, and neck pain, especially in the short term. It can be combined with physical therapy and progressive strength programs to help you move better and recover faster. Mechanistically, acupuncture acts through the nervous system to modulate pain signaling, reduce muscle overactivity, and influence inflammatory pathways, all without relying on medication.
Conclusion
The 2025 evidence map shows that acupuncture may help with common musculoskeletal problems like low back pain, osteoarthritis, neck pain, rheumatoid arthritis, and gout, especially in the short term, with some long-term benefit for low back pain. The overall quality of the included reviews was low to critically low, so results should be interpreted with care and paired with what we see clinically. The practical takeaway is simple. Acupuncture is a low-risk option that can reduce pain, relax overactive muscles, and make it easier to progress your rehab or training. If you want a plan that fits your goals and schedule, we can help you design it and coordinate with your PT or coach.
Ready to Try Acupuncture & Dry Needling?
Whether you’re struggling with acute or chronic pain, acupuncture and dry needling may help restore mobility and reduce pain - quickly and safely.
📍 Conveniently located in New York City
🧠 Experts in trigger point therapy, acupuncture, and dry needling
Book your appointment today with the experts at Morningside Acupuncture, the top-rated acupuncture and dry needling clinic in New York City.
Let us help you move better, feel stronger, and live pain-free.
Related Questions:
-
Yes—reviews in the 2025 evidence map found acupuncture may reduce low back pain in the short term compared with sham, medications, no treatment, and usual care, with some benefits lasting at follow-up. In a few analyses it performed about the same as TENS.
-
Yes—short-term pain relief was consistently better than sham, medications, no treatment, usual care, and waitlist in many reviews. Long-term data were limited but trended positive; some electroacupuncture comparisons to drugs or generic controls were not superior.
-
Mixed—acupuncture outperformed drug therapy and no-treatment controls in some reviews, but was not better than sham in others; long-term data were limited.
-
Often yes in the short term—many reviews showed benefit versus control and usual care, though some electroacupuncture comparisons were similar to sham. Longer-term results looked similar to sham TENS.
-
Promising—electroacupuncture reduced pain versus sham in short-term comparisons, though the number of reviews is smaller, so findings should be viewed as preliminary.
-
Encouraging—acupuncture (including warm needle and electroacupuncture) improved pain versus drug therapy or control in limited reviews. More research would help confirm durability.
-
Some patients feel a change after 1 to 3 visits, especially when muscle tension is a big driver. For most musculoskeletal problems, a trial of once or twice weekly for 4 to 8 weeks is reasonable. We adjust frequency based on irritability, training load, and schedule.
-
Acupuncture is the use of an acupuncture needle and includes hundreds of styles and techniques. Traditional acupuncture refers to styles like TCM and classical acupuncture that rely on acupoints and meridians. Dry needling is an acupuncture style that targets dysfunctional muscle bands and periarticular tender points using an acupuncture needle.
-
Serious adverse events are rare. Most patients have no side effects or experience minor, short-lived soreness or bruising. We screen for contraindications and adapt techniques for sensitive areas and medical conditions.
-
Pain relief may be immediate or build over several sessions. The best way to lock in gains is to combine acupuncture with movement strategies, progressive strength work, and load management. We coordinate with physical therapy and training programs to support this.
-
It depends on the condition and goals. Electroacupuncture can be useful for persistent pain and stubborn muscle guarding because it provides a steady, measurable stimulus. Manual acupuncture is versatile and effective across many presentations. We use the least intrusive option that fits your exam and response.
Sources:
Ang, L., Song, E., Choi, T.-Y., Jun, J. H., Lee, B., Yim, M. H., Lee, H. W., & Lee, M. S. (2025). Effects of acupuncture on musculoskeletal pain: An evidence map. Frontiers in Medicine, 12, 1575226. https://doi.org/10.3389/fmed.2025.1575226
Vickers, A. J., Cronin, A. M., Maschino, A. C., Lewith, G., MacPherson, H., Foster, N. E., et al. (2012). Acupuncture for chronic pain: Individual patient data meta-analysis of 29 randomized controlled trials. Archives of Internal Medicine, 172(19), 1444–1453. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3491930/
Zhao, Z.-Q. (2008). Neural mechanism underlying acupuncture analgesia. Neuroscience Bulletin, 24(3), 125–130. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2752246/
Disclaimer: This web site is intended for educational and informational purposes only. Reading this website does not constitute providing medical advice or any professional services. This information should not be used for diagnosing or treating any health issue or disease. Those seeking medical advice should consult with a licensed physician. Seek the advice of a medical doctor or other qualified health professional for any medical condition. If you think you have a medical emergency, call 911 or go to the emergency room. No acupuncturist-patient relationship is created by reading this website or using the information. Morningside Acupuncture PLLC and its employees and contributors do not make any express or implied representations with respect to the information on this site or its use.